Do you find yourself struggling frequently with IBS symptoms flaring up after having your meals? Don’t worry, you are not alone, and this issue has many ways to alleviate those discomforts. Research has discovered that certain foods (high FODMAPs) can be the culprit of these annoying symptoms. As a dietitian, I’ve noticed the remarkable effects on IBS patients when following a low-FODMAP diet. However, IBS patients finally experienced symptom relief that included (bloating, diarrhea, and gastrointestinal cramps).
Moreover, researchers have revealed more benefits linked to the low-FODMAP diet, so, if you are curious to know more about its benefits, best candidates, and meal plans, continue reading.
What is a Low-FODMAP Diet?
A low-FODMAP diet is a dietary approach designed to alleviate symptoms in individuals with irritable bowel syndrome (IBS) and other gastrointestinal conditions.
What does FODMAP mean?
FODMAP stands for Fermentable, Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
- Fermentable means these carbs get broken down by bacteria in your gut.
- Oligosaccharides are like few sugar chains with just a few links. They are divided into two subgroups, known as fructans and galactans (or galactooligosaccharides)
- Disaccharides are double sugar molecules – It has only one group called lactose.
- Monosaccharides are single sugar molecules called fructose.
- Polyols are sugar alcohols and have sorbitol and mannitol as subgroups.
These compounds can ferment in the gut, leading to symptoms such as bloating, gas, abdominal pain, and diarrhea in susceptible individuals. The low-FODMAP diet involves reducing or eliminating high-FODMAP foods from the diet and then gradually reintroducing them to identify trigger foods.
FODMAP Symptoms
When ingesting FODMAPs, several steps occur that lead to discomfort symptoms for IBS patients:
- Poor Absorption in the Small Intestine: FODMAPs, which include fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, are poorly absorbed in the small intestine. This is due to various factors such as the absence of luminal enzymes capable of breaking down these carbohydrates, the low activity of brush border enzymes like lactase, or the presence of low-capacity epithelial transporters.

Osmotic Effect: Because FODMAPs are not well absorbed, their small molecular size causes an osmotic effect in the small intestine. This osmotic effect draws water (H2O) into the large intestine.

Fermentation by Colonic Microflora: Once in the large intestine, FODMAPs are fermented by colonic microflora, which are the bacteria residing in the colon. During fermentation, these bacteria break down FODMAPs, producing hydrogen (H2) and/or methane gas (CH4).

Fluid and Gas Accumulation: The increase in fluid due to the osmotic effect, along with the production of gas during fermentation, leads to excessive fluid and gas accumulation in the large intestine.


Acute High-FODMAP Symptoms
The combination of increased fluid and gas in the large intestine results in various discomfort symptoms, including:
- Diarrhea: Excessive fluid in the large intestine can lead to diarrhea.
- Bloating: The accumulation of gas in the large intestine causes bloating, a sensation of fullness or tightness in the abdomen.
- Flatulence: The production of gas during fermentation results in flatulence, or passing gas.
- Abdominal Pain: The distension of the intestines due to fluid and gas accumulation can cause abdominal pain.
- Distension: The abdomen may appear visibly swollen or distended due to the excess fluid and gas.
Long-term (Chronic) High-FODMAP Symptoms
Visceral hypersensitivity: A heightened sensitivity to pain or discomfort in your internal organs, such as those found in your chest, abdomen, and pelvic cavity. This phenomenon is a result of advanced glycation and the abundance of gram-negative bacteria in your gut from high FODMAPs.
Essentially, if you have visceral hypersensitivity, even mild pressure or normal bodily functions might trigger pain sensations in these areas because your pain threshold is lower than average.
Overall, the poor absorption of FODMAPs in the small intestine, coupled with their fermentation in the large intestine, leads to discomfort symptoms such as diarrhea, bloating, flatulence, abdominal pain, and distension.
Promise
The low-FODMAP diet is an eating plan aimed at alleviating symptoms of digestive issues, particularly irritable bowel syndrome (IBS), promoting better digestion and strengthening immunity.
Symptoms relief can be achieved by reducing the intake of certain foods with high FODMAP content.
What exactly does a low-FODMAP diet promise upon following it:
- Relief from IBS Digestive Symptoms: The low-FODMAP diet promises to ease symptoms and discomfort associated with digestive issues like irritable bowel syndrome (IBS), offering relief from symptoms such as bloating, gas, and abdominal cramps.
- Support for Gut Health: By cutting down on fermentable carbohydrates, this diet aims to affect the gut microbiome, especially Bifidobacteria. However, the effect on the colonic microbiome is not that significant.
- Encouragement of Healthier Eating: Through its focus on whole, unprocessed foods, the low-FODMAP diet encourages individuals to adopt healthier eating habits, fostering better overall nutrition and well-being.
How to Implement a Low-FODMAP Diet
First, the Low-FODMAP diet plan comprises 3 basic stages. Contrary to what some may think, the FODMAP diet does not apply for a lifetime, but only for 2-6 weeks.
Phase 1: Elimination or Reduction of FODMAPs
Duration: 2 – 8 weeks
Goal: To test the efficacy of a low-FODMAP diet on your symptoms
Induction stage: The stage of stopping foods containing high levels of FODMAPd lasts from 2 weeks to 8 weeks. The goal of this stage is to eliminate symptoms so you can start the second stage.
Action:
- If your body responds positively and symptoms are relieving, proceed to the next phase.
- If there is no response, then return to your original diet.

Phase 2: Reintroduction and Assessment
Duration: 2 – 3 days
Goal: Knowing which FODMAP group exactly causes the symptoms.
At this stage, the nutritionist or your doctor begins to reintroduce FODMAP subgroups individually and monitor the body response.
Action:
- If you do not have new symptoms, increase the amount until these foods become part of your diet without problems. The same applies to the rest of the varieties.
- If you get symptoms after eating these foods, you will refrain from them again until the symptoms disappear and you experiment with another variety.

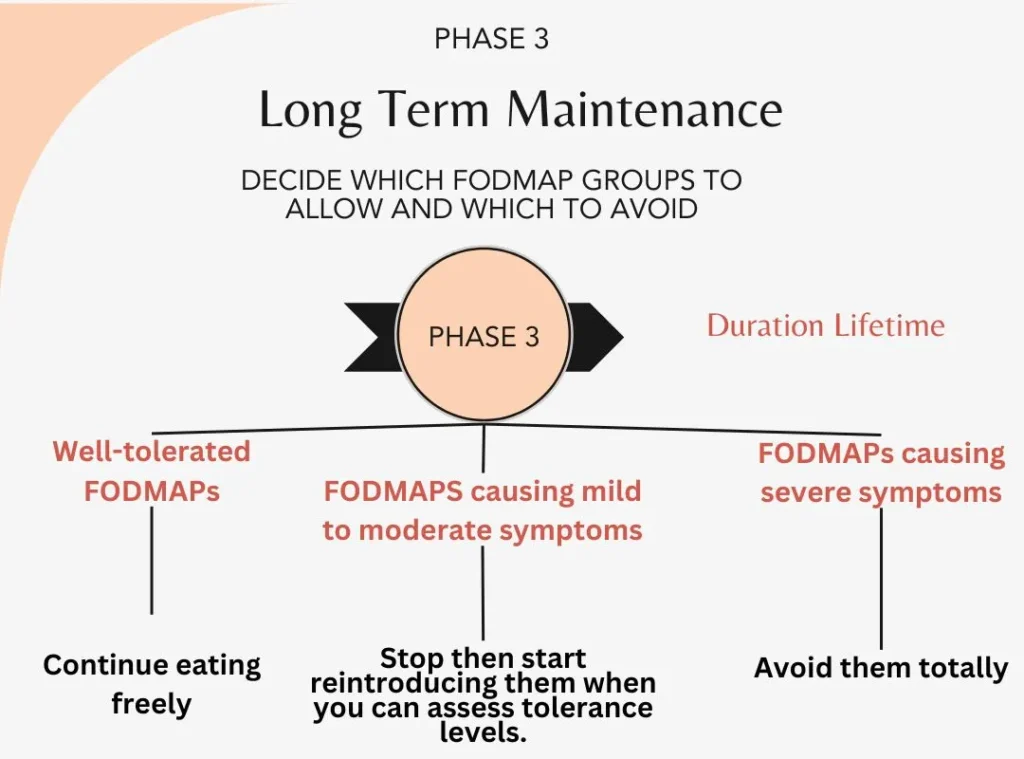
Phase 3: Long Term Maintenance
Duration: Lifetime
Goal: Setting your personalized diet rules based on sensitivity to special items.
After entering the adaptation process and identifying the foods you can eat without problems, both in terms of quantity and type, you will be ready for life with a relatively natural diet.
Your foods following a low-FODMAP diet should be categorized as follows:
- Well-tolerated FODMAPs: Continue eating them freely.
- FODMAPs causing mild-moderate symptoms: try reintroducing them when you can assess tolerance levels.
- FODMAPs causing severe symptoms: Avoid them or eat them lightly. Usually, you will find that these items are few and easy to avoid.
Check out another elimination diet (AIP for auto-immune diseases).
Low-FODMAP Diet Results
Efficacy in Symptom Relief: Studies, including randomized controlled trials and observational studies, have consistently shown that the elimination phase of the low-FODMAP diet provides significant relief for gastrointestinal symptoms in adult patients with irritable bowel syndrome (IBS). Clinical response rates range from 50% to 86%.
Challenges with Maintenance Phase: While the elimination phase’s efficacy is well-established, the success of the maintenance phase (reintroduction of specific FODMAPs) has been less studied due to methodological challenges in designing longer-term interventional studies.
Download our helpful Free Low-FODMAP checklist now that will make it easy for you to:
- Pinpoint and avoid high-FODMAP foods that exacerbate digestive symptoms.
- Reduces bloating, gas, abdominal pain, and diarrhea associated with conditions like IBS.
- Control symptoms and enhance overall well-being.
- Have clear direction on which foods to eliminate and reintroduce during the diet.
- Include alternative low-FODMAP foods for balanced nutrition.
[forminator_form id=”6799″]
Drawbacks of a Low-FODMAP Diet
While dietary therapies like the low-FODMAP diet are often considered safe approaches for managing digestive issues, they are not without risks. In particular, concerns have been raised regarding the inappropriate use of the low-FODMAP diet, its impact on gut microbiota, and the potential for disordered eating behaviors to arise. These issues underscore the need for careful consideration and monitoring when implementing dietary interventions for gastrointestinal disorders.
- Inappropriate Use: Some health professionals may use the low-FODMAP diet as a diagnostic test for irritable bowel syndrome (IBS) instead of following proper diagnostic guidelines. This can lead to misdiagnosis and inappropriate treatment.
- Impact on Gut Microbiota: Restricting certain carbohydrates in the low-FODMAP diet may reduce beneficial gut bacteria, potentially worsening symptoms in the long term. This alteration in gut bacteria composition could have unknown health implications.
- Risk of Disordered Eating: Individuals with gastrointestinal disorders who undergo
dietary changes, including the low-FODMAP diet, may be at increased risk of developing disordered eating behaviors. This can lead to anxiety around food, social isolation, and orthorexia nervosa, a condition characterized by an obsessive focus on healthy eating.
In a study involving almost a thousand people with Irritable Bowel Syndrome (IBS), researchers looked at 13 different trials. They found that following a low FODMAP diet – which focuses on specific types of carbs – was the most effective way to ease IBS symptoms compared to sticking with regular eating habits.
This diet also did a better job at reducing the severity of tummy pain, and bloating, and helping with regular bathroom trips. Specifically, it worked better than advice from the British Dietetic Association (BDA) and the National Institute for Health and Care Excellence (NICE) in easing bloating. Other dietary tips from BDA/NICE didn’t prove to be better than anything else.
Foods to Avoid on Low-FODMAP Diet Phase 1 (Elimination phase)
Although the FODMAP list includes a lot of varieties, there are still many foods that can be eaten.
| F | Fermented by bacteria in your intestinal flora | ||
| O | Oligo-saccharides | fructose and galactose | wheat, barley, rye, onions, leeks, the white part of lettuce, garlic, onions, artichokes, beets, fennel, peas, dandelion, pistachios, cashews, legumes, lentils, chickpeas. |
| D | Disaccharides | lactose | Milk, custard, ice cream, yogurt |
| M | mono-saccharides | fructose | Mangoes, Apples, cherries, melons, asparagus, peas, pears, honey, high fructose corn syrup. |
| A | And | ||
| P | Polysaccharides | sorbitol, mannitol | Apples, pears, apricots, cherries, nectarines, peaches, watermelons, and melons. Mushrooms, cauliflower, gum, artificial sweets, and sweets. |
- Fruits: Apple, clingstone peach, mango, nashi pear, pear, sugar snap pea, tinned fruit in natural juice, watermelon, custard apple, persimmon, rambutan, white peach, apricot, avocado, cherry, longan, lychee, nectarine, plum, and prune.
- Honey Sweeteners: Fructose and high-fructose corn syrup.
- Large Total Fructose Dose: Concentrated fruit sources, large servings of fruit, dried fruit, and fruit juice.
- Milk: Regular and low-fat cow milk, goat milk, sheep milk, and ice cream.
- Yogurts: Regular and low-fat yogurts.
- Cheeses: Soft and fresh cheeses.
- Vegetables: Artichoke, asparagus, beetroot, broccoli, Brussels sprout, cabbage, cauliflower, fennel, garlic, leek, mushroom, okra, onion, pea, shallot, and snow pea.
- Cereals: Rye cereals and wheat cereals when eaten in large amounts (e.g., biscuit, bread, couscous, cracker, pasta).
- Legumes: Baked bean, chickpea, lentil, and red kidney bean.Sweeteners: Isomalt, maltitol, mannitol, sorbitol, xylitol, and other sweeteners ending in “-ol”.
Low-FODMAP Foods Allowed on Phase 1 (Elimination phase)
- Fruits: Banana, blueberry, cantaloupe, carambola, durian, grape, grapefruit, honeydew melon, kiwi, lemon, lime, orange, passion fruit, pawpaw, raspberry, strawberry, tangelo.
- Honey Substitutes: Golden syrup, maple syrup.
- Sweeteners: Any sweeteners except polyols.
- Milk: Lactose-free milk, rice milk.
- Meal Replacement shakes specified for low-FODMAP diet.
- Ice Cream Substitutes: Gelato, sorbet.
- Yogurts: Lactose-free yogurts.
- Cheeses: Hard cheeses.
- Vegetables: Bamboo shoot, bok choy, capsicum, carrot, celery, chives, choko, choy sum, corn, eggplant, green bean, lettuce, parsnip, pumpkin, silverbeet, spring onion (green part only).
- Onion/Garlic Substitutes: Garlic-infused oil.
- Cereals: Gluten-free and spelled bread/cereal products.
- Fruit: Tomato.
- Sweeteners: Glucose, sugar (sucrose), other artificial sweeteners not ending in “-ol”.

Low-FODMAP Diet Shopping List for Initial Phase (2-8 Weeks)
Here is a sample shopping list for 2-8 weeks of low FODMAP foods, with non-FODMAP items included:
- Fruits: Bananas, blueberries, cantaloupe melon, grapes, oranges, strawberries
- Vegetables: Bell pepper (capsicum), carrots, lettuce, cherry tomatoes
- Dairy: Lactose-free milk, lactose-free yogurt, hard cheese
- Other: Golden syrup, maple syrup, glucose, sugar (sucrose), gelato, sorbet, garlic-infused oil, gluten-free bread/cereal products, spelled bread/cereal products
Additionally, you can include non-FODMAP proteins such as chicken, turkey, fish, eggs, tofu, and seafood to complete your meals. Remember to choose lean cuts of meat and avoid processed meats to keep your meals low FODMAP and healthy.
Low-FODMAP Diet Contraindications
Low-FODMAP diet is just like any other diet, as it might not be suitable for anyone as it’s a bit complex.
If you are with any of these contraindications, a modified approach or alternative treatment plan may be necessary. It’s crucial to assess your suitability and consider alternative options to ensure safe and effective management.
- Having Difficulty Understanding or Applying the Diet: If you find it hard to grasp or follow the complexities of the low FODMAP diet, it may not be suitable for you.
- Already Restricted Diet: If you are already on a highly restricted diet due to various reasons, adopting the low FODMAP diet might not be a good idea. It might lead to further limitations and potential nutritional deficiencies.
- Unexplained Weight Loss or Low BMI: If you experienced unexplained weight loss after starting a low-FODMAP diet or already have a low Body Mass Index (BMI), then, it might not be suitable for you. However, if you decide to proceed with it, you should approach the low FODMAP diet cautiously, as it may exacerbate nutritional deficiencies.
- Eating Disorders: Those with eating disorders such as avoidant restrictive food intake disorder or orthorexia nervosa should avoid the low FODMAP diet as it may contribute to unhealthy eating behaviors.
- Constipation-Predominant Symptoms: Having constipation-predominant symptoms with IBS makes the low FODMAP diet not the best approach and could exacerbate the issue.
Alternatives to Low-FODMAP Diet
Traditional IBS Diet
Evidence suggests that many IBS patients can reintroduce FODMAPs after initially reducing them, maintaining good symptom control with only mild restriction. This suggests a broader change in diet may be beneficial.
Gut-Directed Hypnotherapy
Randomized trials show gut-directed hypnotherapy to be as effective as the low-FODMAP diet for relieving gastrointestinal symptoms in IBS patients. It may even offer superior improvements in psychological well-being.
Gluten-Free Diet (GFD)
While no comparative studies exist between low-FODMAP and GFD, observational reports suggest similar response rates. However, the effectiveness of symptom relief with a gluten-free diet may be due to reduced FODMAP intake rather than solely gluten avoidance.
Non-Celiac Gluten Sensitivity (NCGS)
Evidence suggests that symptoms in patients labeled with NCGS may be more related to FODMAPs than gluten. For most IBS patients, identifying trigger foods and gradually reintroducing them is crucial to minimizing dietary restrictions and associated risks.
Download our helpful Free Low-FODMAP checklist now!!
[forminator_form id=”6799″]

FAQs
Why you shouldn’t follow a low-FODMAP diet for the long term?
It might cause nutritional deficiencies and may alter the gut microbiome.
While a low-FODMAP diet can be effective for managing Irritable Bowel Syndrome (IBS) symptoms in the short term, it’s not advisable to follow it for the long term due to potential drawbacks:
- Long-term adherence to a low-FODMAP diet may lead to nutritional deficiencies.
- Prolonged restriction of fermentable carbohydrates can alter the gut microbiome.
However, recent research shows that following all phases of the low-FODMAP diet under a dietitian’s supervision can be safe and effective for managing IBS symptoms.
It’s crucial to consult with a healthcare professional before committing to any long-term dietary changes.
Why doesn’t the low FODMAP diet work with me?
Not sensitive to FODMAPs, cheating on the low FODMAP diet, or your symptoms aren’t caused by IBS.
Despite positive results, and that it is one of the treatment methods that a doctor may use with the patient to treat irritable bowel syndrome, some people may not feel better after following it.
But be aware that you fall into one of these mistakes, as it may be the reason the low FODMAP diet doesn’t work with you :
- Failure to check the ingredients in processed foods: Even though eating processed foods isn’t allowed in the initial phase, sometimes you might be convinced that some are free from FODMAPs. Unfortunately, these products may contain additives that may be among the high FODMAP foods.
- FODMAP insensitivity: While this diet works wonders for many with IBS, it’s not a silver bullet for everyone. Studies suggest that around 50 to 80% of patients with IBS find relief during the initial phase of the diet. But that means there are still many, about 20-50%, who don’t see the same results. It’s all about comparing how you felt before and after those first few weeks to gauge if it’s making a difference for you.
- Follow an inaccurate low-FODMAP list or not strict enough: Sometimes, the reason the low-FODMAP diet falls short is that it hasn’t been followed as strictly as it needs to be. Maybe you accidentally snuck in some high FODMAP foods without realizing it, or perhaps sticking to the restrictions proved tougher than expected. A seasoned dietitian familiar with IBS can take a closer look at your eating habits to see if there’s room for improvement. They’ll examine things like portion sizes, dining out tendencies, and whether you’ve been inadvertently indulging in high FODMAP ingredients lurking in processed foods.
- Your Symptoms Aren’t Caused by IBS: It’s also possible that there’s more than just IBS at play here. Conditions like inflammatory bowel disease, coeliac disease, or endometriosis can masquerade as IBS and lead to similar symptoms. If these haven’t been ruled out yet, it might be worth having a chat with your GP or a gastroenterologist to explore further testing.
Does the Low-FODMAP Diet have a positive effect on Chron’s Disease?
Yes, the low-FODMAP Diet has a positive effect on Chron’s disease, but still further research is needed.
Some research suggests that the low-FODMAP diet could be beneficial for managing gastrointestinal symptoms in CD patients. However, further research is required to compare its effectiveness with other dietary approaches, especially over the long term.
Is the low-FODMAP diet Worth it?
Despite its effectiveness, there’s ongoing debate regarding whether the low-FODMAP diet should be considered a first-line therapy for IBS. Critics raise concerns about study design, placebo effect, blinding, and sample sizes which may lead to inaccurate results.
Additionally, there’s debate about how the diet’s efficacy relates to different subgroups of IBS based on predominant bowel habits.
Despite criticisms, the weight of evidence from various studies supports the efficacy of the low-FODMAP diet in relieving gastrointestinal symptoms in IBS patients. However, it’s important to consider these criticisms when evaluating the quality and strength of the study results.
Download our helpful Free Low-FODMAP checklist now!!
[forminator_form id=”6799″]
Will a low-FODMAP diet benefit me if I’m not diagnosed with IBS?
No, a low FODMAP diet won’t benefit you if you aren’t diagnosed with IBS.
The low FODMAP diet is specifically designed for patients with medically diagnosed IBS. If you haven’t seen a doctor about your gut issues, it’s not the right time to start following this diet. There are several conditions out there with symptoms that look a lot like IBS, such as coeliac disease, inflammatory bowel disease, endometriosis, and even bowel cancer.
Self-diagnosing yourself with IBS isn’t a good idea. Instead, make an appointment with your doctor. They’ll take a close look at your symptoms, possibly run some tests, and give you a proper diagnosis if it’s IBS. Once you have that clarity, then you and your doctor can discuss whether the low FODMAP diet is the way to go.
In wrapping up, the duration of FODMAP symptoms is a nuanced topic with individual variability. Understanding the duration FODMAP symptoms take to vanish is crucial for managing digestive discomfort effectively. By identifying trigger foods, working closely with healthcare professionals, and implementing personalized management strategies, individuals can take control of their digestive health journey with confidence and clarity.
