If you’re waking up suddenly with itching, anxiety, a racing heart, or feeling “wired but tired,” there’s a good chance you’re experiencing histamine dump at night symptoms. Many people don’t realize that histamine isn’t just an allergy chemical — it’s also tied to your sleep cycles, gut health, hormones, and even stress levels. So when histamine builds up and releases in a wave, especially around 3 a.m., it can jolt you awake out of nowhere.
Maybe this sounds familiar: You fall asleep normally, then wake up sweaty or restless… you can’t settle down… your thoughts are racing… or your skin feels prickly. It’s frustrating because nothing looks wrong — but your body is stuck in “alert mode,” not “sleep mode.”
Research shows that histamine levels naturally rise at night, and if your body struggles to clear histamine properly, that rise becomes a dump, leading to symptoms like increased heart rate, insomnia, stomach discomfort, or anxiety spikes.¹ ² These episodes are more common in people with gut inflammation, high stress, or nutrient deficiencies that affect DAO — the enzyme that clears histamine.
The good news? You’re not imagining these symptoms, you’re not “overreacting,” and there are ways to calm them. Understanding what a histamine dump is — and how to support your body so histamine clears more efficiently — is the first step.
You’re in the right place. Let’s break this down in a simple, supportive way that actually makes sense.
Contents
- 0.1 What a Histamine Dump Really Is and Why It Happens at Night
- 0.2 The Hidden Nighttime Histamine Symptoms Most People Don’t Recognize
- 0.2.1 Your Body Releases More Histamine at Night Than You Think
- 0.2.2 Your Liver and Nervous System Work Hardest Between 1–3 AM
- 0.2.3 Stress Makes Nighttime Histamine Spikes Worse
- 0.2.4 Gut Issues Can Trigger Nighttime Histamine Dumps Too
- 0.2.5 The Symptoms Most People Don’t Connect to Histamine Surges
- 0.2.6 Why You Only Notice It At Night (Not During the Day)
- 0.3 Why Histamine Spikes Often Happen Around 3 a.m.
- 0.3.1 Your Circadian Rhythm Naturally Raises Histamine Overnight
- 0.3.2 Your Cortisol Is at Its Lowest Around 3 a.m. (And That Matters)
- 0.3.3 Your Liver’s “Night Shift” Kicks In
- 0.3.4 Blood Sugar Dips Can Trigger a Histamine Release
- 0.3.5 Your Gut Slows Down at Night (Allowing Histamine to Accumulate)
- 0.3.6 Melatonin and Histamine Are Linked More Than You Think
- 0.3.7 You Feel It Most at 3 a.m. Because Everything Else Is Quiet
- 0.4 How Stress and Cortisol Make Nighttime Histamine Surges Worse
- 1 Feeling Stressed Lately?
- 1.0.1 Chronic Stress Keeps Your Body in “Alert Mode” All Day
- 1.0.2 Cortisol Normally Keeps Histamine Calm — Until It Can’t
- 1.0.3 The Nighttime Cortisol Drop Makes Histamine Louder
- 1.0.4 Stress Raises Adrenaline — and Adrenaline Triggers Histamine
- 1.0.5 Stress Weakens the Gut, Making You More Histamine-Sensitive
- 1.0.6 Stress Disrupts Sleep — and Poor Sleep Raises Histamine
- 1.0.7 The Takeaway: Stress Doesn’t Just Make Symptoms Worse — It Changes Your Histamine Threshold
- 1.1 The Gut–Sleep Link and How Poor Histamine Breakdown Disrupts Rest
- 1.1.1 Your Gut Is Where Histamine Gets Cleared — or Builds Up
- 1.1.2 Why Histamine Feels Worse at Night
- 1.1.3 Gut Inflammation Signals the Brain and Disrupts Melatonin
- 1.1.4 When Gut Bacteria Are Off, Histamine Goes Up
- 1.1.5 Why You Wake Up Bloated or Gassy at 3 a.m.
- 1.1.6 The Takeaway: Your Gut Health Determines Your Sleep Quality
- 1.2 Simple Ways to Calm a Nighttime Histamine Dump Naturally
- 1.2.1 Hydrate Slowly to Help Your Body Clear Histamine
- 1.2.2 Use Gentle Deep Breathing to Settle Your Nervous System
- 1.2.3 Cool the Room Slightly to Reduce Histamine-Related Heat
- 1.2.4 Avoid Checking Your Phone — Light Triggers More Histamine
- 1.2.5 Try a Gentle Position Change
- 1.2.6 Use Soothing, Low-Histamine Snacks if You Feel Weak
- 1.2.7 Release Body Tension With a Quick “Reset” Stretch
- 1.2.8 Remind Yourself: This Is a Histamine Surge — Not an Emergency
- 1.3 Frequently Asked Questions
- 1.3.1 Can a nighttime histamine dump happen even if I eat low-histamine foods all day?
- 1.3.2 Why do I get itchy skin only at night and not during the day?
- 1.3.3 Can a histamine dump wake me from deep sleep without any digestive symptoms?
- 1.3.4 Is it normal to feel wired but exhausted after a nighttime histamine spike?
- 1.3.5 Can dehydration make nighttime histamine symptoms worse?
- 1.3.6 Does sleeping in a warmer room increase the chance of a histamine dump?
- 1.3.7 Can certain supplements make nighttime histamine spikes worse?
- 1.3.8 Can I have a histamine dump even if my allergy tests come back normal?
- 1.3.9 Does poor sleep itself increase nighttime histamine reactions?
- 1.3.10 Can my menstrual cycle affect nighttime histamine symptoms?
- 1.4 Conclusion
What a Histamine Dump Really Is and Why It Happens at Night
Your Body Uses Histamine for More Than Allergies
When people hear “histamine,” they usually think of allergies — sneezing, itching, watery eyes. But histamine is actually a neurotransmitter, meaning your brain uses it to regulate wakefulness, digestion, and immune responses.
This is why histamine spikes can make you feel suddenly alert, restless, or uncomfortable at night. Research shows that histamine-producing neurons in the brain remain highly active during wakefulness and naturally quiet down during sleep. When they don’t, the body feels “on” when it’s supposed to be resting.¹
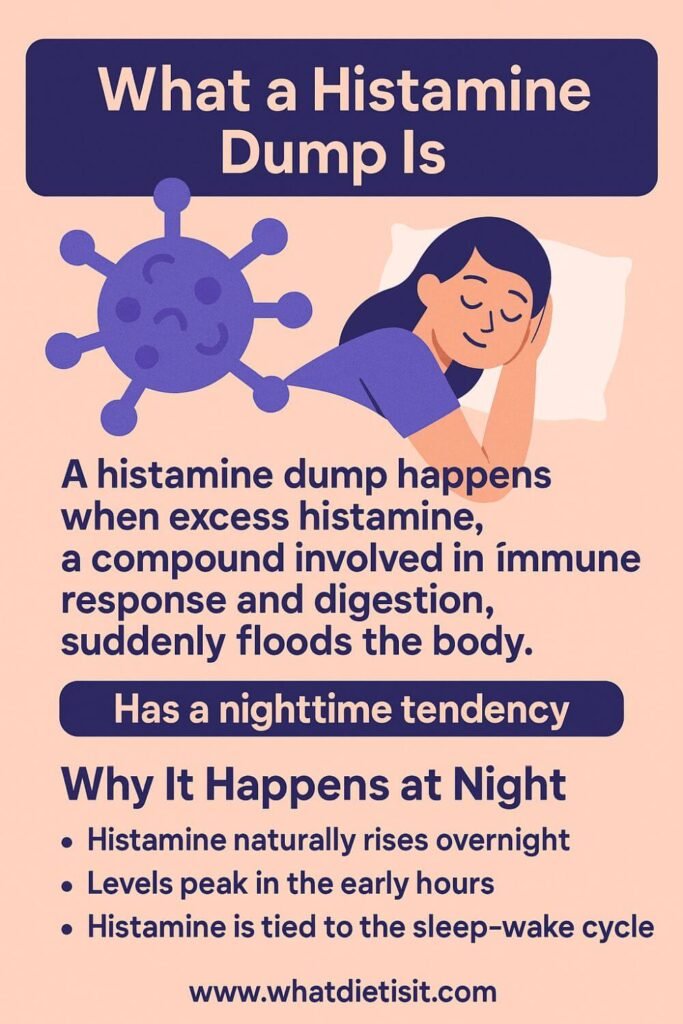
What a “Histamine Dump” Actually Means
A “histamine dump” isn’t an official medical term, but it accurately describes what happens when your body releases a large pulse of histamine at once — usually because your system is overwhelmed, inflamed, or unable to break histamine down efficiently.
Enzymes like DAO (diamine oxidase) and HNMT are responsible for clearing histamine, and when they slow down (from stress, gut imbalance, nutrient deficiencies, or heavy histamine foods), histamine builds up until your body releases it suddenly.²
That sudden release is what wakes you up with symptoms like racing heart, itching, warmth, anxiety, or a “wired but tired” feeling.
Why It Happens More Often at Night
Nighttime is when your body switches from “doing” to “repairing.” Unfortunately, this is also when histamine can spike.
Here’s why:
- DAO enzyme activity naturally drops at night, so your body clears histamine more slowly.³
- Melatonin and histamine work in opposite directions — when histamine is high, melatonin drops, which interrupts sleep.
- Digestion slows while sleeping, so histamine from food lingers in the gut longer.
- Cortisol dips at night, and low cortisol can increase mast-cell activity (mast cells release histamine).
This combination creates the perfect environment for a histamine surge to hit during the hours when your immune and digestive systems are most active internally — often between 1 a.m. and 4 a.m.
If you’re waking up around 3 a.m. with symptoms, your body isn’t malfunctioning — it’s overwhelmed. And your nervous system is simply responding to that histamine spike.
Why You’re Not Imagining These Symptoms
Many people second-guess themselves:
“Why did I wake up with anxiety for no reason?”
“Why does my skin itch more at night?”
“Why do symptoms hit only when I’m trying to sleep?”
There is a reason — and it’s biological. Peer-reviewed research consistently shows that histamine influences alertness, sleep regulation, heart rate, gut motility, and inflammation.¹ ²
So when histamine rises at night, your body acts like it’s morning again — even though you desperately want to sleep.
You’re not imagining it.
You’re not “being dramatic.”
Your body is reacting to a chemical signal that has a real, measurable effect on your sleep and symptoms.

The Hidden Nighttime Histamine Symptoms Most People Don’t Recognize
If you keep waking up at night with symptoms that feel “random” — a racing heartbeat, sudden warmth, anxiety that hits out of nowhere, or itchy skin the moment your head hits the pillow — you’re not imagining it. These episodes are often signs of a nighttime histamine dump, and they’re much more common than people realize.
You’re not overreacting. Your body is trying to tell you something.
Histamine isn’t just about allergies — it’s a neurotransmitter, a digestion regulator, and a wakefulness signal. And at night, when your body is supposed to calm down, a buildup of histamine can do the exact opposite.
Let’s break down what’s really happening inside your body.

Your Body Releases More Histamine at Night Than You Think
Even if you don’t have allergies, your body naturally produces histamine around the clock — but the release follows a circadian rhythm. Research shows that histamine levels often peak at night, especially during the early sleep cycles, because mast cells (your histamine-releasing immune cells) become more active after dark.
So if you already have extra histamine built up from food, stress, or gut issues… that nighttime peak can feel like an internal “alarm” going off.
This is why so many people wake up between 1–3 AM with symptoms they can’t explain.
Your Liver and Nervous System Work Hardest Between 1–3 AM
Traditional medicine and modern research surprisingly agree on one thing:
your liver does a lot of its detoxification work deep into the night.
And histamine clearance depends heavily on liver enzymes — especially DAO (diamine oxidase) and HNMT. If these enzymes are sluggish from stress, nutrient deficiencies, or inflammation, histamine lingers longer in your system.
So when your liver starts clearing hormones, toxins, and metabolic waste around 2 AM, you may get a sudden surge of symptoms like:
- A loud, pounding heartbeat
- Warmth or night sweats
- A “wired-but-tired” feeling
- Panic-like sensations
- Bloating or sudden gas
This isn’t anxiety.
This is physiology.
Stress Makes Nighttime Histamine Spikes Worse
If you feel worse on days when you’re stressed, there’s a reason.
Cortisol — your stress hormone — usually drops at night so you can sleep. But when cortisol is dysregulated (high in the evening or crashes suddenly), it can trigger mast cells to release more histamine.
This is why people with:
- A stressful week
- Burnout
- Overthinking at night
- Blood sugar crashes
- Hormonal fluctuations
often notice symptoms becoming stronger in the dark.
Your body is not “being dramatic.”
It’s responding to overload.
Gut Issues Can Trigger Nighttime Histamine Dumps Too
About 70% of your immune cells live in your gut — including the mast cells that release histamine.
If you’re dealing with gut inflammation, SIBO, IBS, leaky gut, or even mild food sensitivities, your gut may release histamine more easily.
Because digestion slows at night, any histamine left from dinner or poor digestion earlier in the day can trigger:
- Cramping
- Nausea
- Bloating that suddenly appears at bedtime
- Acid reflux
- Restless sleep
It’s not “just your stomach acting up.”
It’s your immune system reacting when your gut is quiet enough for you to notice it.
The Symptoms Most People Don’t Connect to Histamine Surges
Many of the patients in mast cell or histamine research report symptoms they never realized were histamine-related.
You may recognize some of them:
• Heart pounding when you lie down
Histamine widens blood vessels, which increases heart workload temporarily.
• Sharp waves of anxiety or fear at night
Histamine activates wakefulness centers in the brain — it’s literally stimulating.
• Itching, crawling sensations, or skin heat
Mast cells in the skin dump histamine at night, especially after a warm shower.
• Sudden bloating or gas before sleep
Histamine influences gastric acid and gut motility.
• Waking with a sense of “something is wrong”
This is a neurological histamine surge — not a psychological issue.
• Congestion or throat tightness after lying down
Histamine causes swelling of mucous membranes.
If these symptoms sound familiar, I promise you’re not alone — and you’re not imagining it.
Why You Only Notice It At Night (Not During the Day)
During the day, cortisol is higher, your digestion is active, and your brain is stimulated.
All of that can mask histamine buildup.
But at night — when everything slows down — the histamine becomes louder.
Many people feel perfectly normal all day and suddenly “crash” at bedtime.
That’s not inconsistency — that’s your biology revealing what it was holding back.
Why Histamine Spikes Often Happen Around 3 a.m.
If you’re waking up at 3 a.m. feeling wired, anxious, sweaty, hungry, bloated, restless, or like your heart suddenly turned up the volume — it’s not “just stress,” and you’re not imagining it.
Many people experience histamine dumps during this exact time window, and there are real biological reasons behind it.
Let’s break them down so you can understand what your body is actually doing.
Your Circadian Rhythm Naturally Raises Histamine Overnight
Histamine follows a daily rhythm.
During the night — especially between midnight and 4 a.m. — your mast cells release more histamine by design.
Researchers believe this happens because:
- Histamine helps regulate sleep–wake transitions
- Immune surveillance increases during deep sleep
- Mast cells become more reactive when cortisol is low
So if you’re already histamine-sensitive, this nighttime surge can feel like a “mini-storm” inside your body.
Your Cortisol Is at Its Lowest Around 3 a.m. (And That Matters)
Cortisol (your stress-buffering hormone) naturally reaches its lowest point between 2–4 a.m.
That timing is important because:
- Cortisol suppresses mast-cell histamine release
- When cortisol drops, histamine becomes more active
- Low cortisol = higher sensitivity to symptoms
This is why the same foods that felt “fine” during the day can suddenly bother you at night.
If you’ve been stressed, burnt out, or dealing with adrenal dysregulation, this drop feels even more extreme — and histamine becomes louder.
Your Liver’s “Night Shift” Kicks In
Your liver handles a big part of histamine clearance through enzymes like DAO and HNMT.
But here’s the twist:
Your liver also does its deep detox work around 1–3 a.m.
If your liver is processing:
- Hormones
- Medication byproducts
- Blood sugar fluctuations
- Alcohol
- Histamine from food
…you can end up with a temporary “backup” that feels like:
- Heat waves
- Heart racing
- Night sweats
- Restlessness
Many people mistake this as anxiety — it’s often just physiology.
Blood Sugar Dips Can Trigger a Histamine Release
A lot of people who wake up at 3 a.m. notice something else:
You feel wide awake — almost panicked.
Often this happens because your blood sugar dropped too low during sleep.
When that happens, your body releases:
- Adrenaline
- Cortisol
- And yes — histamine
This combination is the perfect recipe for a 3 a.m. “alert” state.
If you wake up hungry, shaky, or with a pounding heart, blood sugar instability may be the hidden cause.
Your Gut Slows Down at Night (Allowing Histamine to Accumulate)
At night, digestion slows dramatically.
If you ate:
- A high-histamine dinner
- Leftovers
- Fermented foods
- Spices
- Tomatoes
- Chocolate
- Aged cheeses
- Certain medications
…your gut may not fully process them until hours later.
That slow breakdown can cause histamine to leak into the bloodstream while you sleep.
This delayed wave often hits around — you guessed it — 3 a.m.
Melatonin and Histamine Are Linked More Than You Think
Melatonin and histamine are opposites in many ways:
- Melatonin calms mast cells
- Histamine activates wakefulness
If melatonin is low (from screens, stress, late nights, or poor sleep routines), histamine becomes more dominant.
This makes nighttime spikes stronger and more noticeable.
You Feel It Most at 3 a.m. Because Everything Else Is Quiet
During the day:
- You’re busy
- Adrenaline is higher
- Your digestion is active
- You’re distracted
At night — especially after your first sleep cycle — there’s nothing to “hide” the symptoms.
What you experience at 3 a.m. is not sudden.
It’s simply the moment your body becomes quiet enough to feel the histamine already building.
How Stress and Cortisol Make Nighttime Histamine Surges Worse
If your nighttime symptoms get dramatically worse during stressful weeks — waking up sweaty, wired at 3 a.m., heart racing, itchy, bloated, or unable to fall back asleep — it isn’t “just anxiety.”
There is a very real biochemical loop between stress → cortisol → histamine, and that loop becomes most noticeable at night.
Let’s break it down so it finally makes sense.
Feeling Stressed Lately?
Take our quick and free stress quiz to discover your current stress level and get personalized wellness tips based on your results.
Take the Free QuizChronic Stress Keeps Your Body in “Alert Mode” All Day
When your brain thinks you’re under stress, it sends signals that activate your sympathetic nervous system — the same system that prepares you to fight or run.
And here’s the part most people don’t know:
Mast cells — the cells that release histamine — also respond directly to stress hormones.
So when you’re stressed:
- Mast cells become more reactive
- They release more histamine
- They respond more strongly to foods, smells, temperature, and hormones
This means the same meal or environment that felt fine last month may suddenly cause symptoms during a stressful week.
Cortisol Normally Keeps Histamine Calm — Until It Can’t
Cortisol isn’t just a “stress hormone.”
It has another job: keeping histamine under control.
During the day, cortisol naturally:
- Reduces mast-cell overactivity
- Helps stabilize inflammation
- Regulates blood sugar
- Keeps the nervous system balanced
But stress flips the script.
If you’ve been under chronic stress (not sleeping well, burnout, emotional overload, overworking), your cortisol pattern becomes irregular:
- Too high at the wrong time
- Too low when you need it
- “Flatlined” throughout the day
- Spiking randomly
Once cortisol becomes dysregulated, it loses the ability to suppress histamine — especially at night.
The Nighttime Cortisol Drop Makes Histamine Louder
Cortisol always reaches its lowest point between 2–4 a.m.
This drop is normal — but when you’re stressed, it becomes extreme.
And this is exactly when most people feel histamine symptoms.
Because when cortisol drops:
- Histamine rises
- Mast cells activate more easily
- Blood pressure and heart rate become less stable
- Inflammation becomes more noticeable
- Your nervous system becomes hypersensitive
This is why you might wake up at 3 a.m. feeling:
- Hot
- Restless
- Itchy
- Hungry
- Overwhelmed
- Heart pounding
- Unable to calm down
It’s not “in your head.”
It’s your physiology responding to an unbuffered histamine wave.
Stress Raises Adrenaline — and Adrenaline Triggers Histamine
When cortisol is unstable, your body compensates with adrenaline.
Adrenaline is a powerful mast-cell activator.
During the night, adrenaline surges can create:
- Sudden racing heart
- Jumps of nervous energy
- Hot flashes
- Pounding in the chest
- A sense of dread or alertness
- Waking up fully awake with no reason
If this happens around 3 a.m., histamine and adrenaline are working together — not against you.
Stress Weakens the Gut, Making You More Histamine-Sensitive
Chronic stress damages the gut lining and reduces DAO production — the enzyme responsible for breaking down histamine.
This means:
- You react to more foods
- You clear histamine more slowly
- Your nighttime symptoms intensify
- Dinner choices hit harder during sleep
Even “healthy” foods can trigger a nighttime histamine dump when the gut is under stress.
Stress Disrupts Sleep — and Poor Sleep Raises Histamine
Histamine is your “wakefulness” neurotransmitter.
So when stress disrupts sleep, histamine increases even more.
If you’ve been:
- Staying up late
- Waking up often
- Sleeping lightly
- Feeling wired but tired
…your brain may be releasing histamine as compensation.
This creates the cycle many people get stuck in:
Stress → poor sleep → more histamine → worse sleep → more stress.

The Takeaway: Stress Doesn’t Just Make Symptoms Worse — It Changes Your Histamine Threshold
If your nighttime symptoms become unpredictable or worsen dramatically during stressful periods, it’s because stress is rewiring the way your body handles histamine.
You are not exaggerating.
Your body is not weak.
It is reacting to a real physiological imbalance — not a psychological one.
The Gut–Sleep Link and How Poor Histamine Breakdown Disrupts Rest
If your nights feel unpredictable — some evenings you fall asleep easily, and other nights you’re wide awake, wired, bloated, itchy, or uncomfortable — your gut may be the missing piece.
Most people don’t realize that the gut controls far more than digestion; it also regulates histamine, neurotransmitters, and the chemicals that help you fall asleep and stay asleep.
And when the gut is irritated, inflamed, or not breaking down histamine properly, your sleep becomes the first thing to suffer.
Let’s walk through this in a way that finally makes sense.
Your Gut Is Where Histamine Gets Cleared — or Builds Up
Your intestines produce an enzyme called DAO (diamine oxidase) — this is your main tool for breaking down histamine from food and from your body.
When the gut lining is healthy, DAO works effectively, and histamine stays balanced.
But when the gut is irritated by:
- Stress
- Processed foods
- Antibiotics
- Food sensitivities
- SIBO
- Infections
- Low stomach acid
…the gut lining becomes inflamed and produces less DAO.
Less DAO = more circulating histamine, especially at night when your body is resting and detoxing.
This is why gut issues often show up as:
- Overnight bloating
- Burning stomach
- Nausea at night
- Sudden itchiness
- Gas at 2–4 a.m.
- Waking up feeling “wired” instead of sleepy
It’s not random — it’s histamine your body couldn’t process.
Why Histamine Feels Worse at Night
Histamine isn’t just an allergy chemical — it’s a wakefulness neurotransmitter.
When histamine is high:
- Your brain becomes alert
- Your nervous system activates
- Your heart rate increases
- Your muscles tense
- Your breathing becomes shallow
- You can’t fully relax
During the day, cortisol helps keep histamine under control.
But cortisol drops naturally at night — especially around 2–4 a.m.
Without cortisol to balance it, histamine “speaks louder.”
If your gut isn’t breaking histamine down efficiently, that nighttime low-cortisol window becomes the perfect time for a histamine surge.
You feel it as:
- A sudden wake-up around 3 a.m.
- Night sweats
- A racing heart
- Restlessness
- Panic-like sensations
- Hot skin or flushing
- Itching or tingling
- Nose congestion
- Weird vivid dreams
This is your brain and gut trying to offload histamine while your body is supposed to be sleeping.
Gut Inflammation Signals the Brain and Disrupts Melatonin
Your gut produces over 90% of your serotonin, which your body converts into melatonin — your sleep hormone.
So when the gut is inflamed or stressed:
- Serotonin becomes unstable
- Melatonin production drops
- Sleep becomes fragmented
- You wake up unrefreshed
- Falling asleep takes longer
Research also shows that gut inflammation increases the release of cytokines (immune messengers) that directly suppress melatonin production.
So if your gut is overactive, your sleep becomes underactive.
When Gut Bacteria Are Off, Histamine Goes Up
Your gut microbiome also plays a major role in histamine balance.
Some bacteria produce histamine, while others break it down.
When your gut is imbalanced (due to stress, antibiotics, or diet):
- Histamine-producing bacteria increase
- Histamine-breaking bacteria decrease
- Gas and bloating worsen at night
- Food reactions intensify
- Sleep becomes lighter and more anxious
This is why some people can eat the same meal for years, then suddenly start reacting to it when their gut state changes.
Why You Wake Up Bloated or Gassy at 3 a.m.
Your digestive system goes into maintenance mode overnight.
If your gut is struggling, night is when symptoms get loudest:
- Food is fermenting in the intestines
- Bacteria are releasing histamine
- Gas is building up
- DAO is low
- Cortisol is low
- Histamine is high
And that’s the exact formula that wakes you up in discomfort.
You’re not imagining it.
Your body is trying to get your attention.
The Takeaway: Your Gut Health Determines Your Sleep Quality
If you’re dealing with histamine-related night symptoms — especially the 3 a.m. wake-up — your gut is likely involved.
Improving gut health is one of the fastest ways to reduce nighttime histamine surges and restore predictable sleep.
Simple Ways to Calm a Nighttime Histamine Dump Naturally
When you’re wide awake at 2 or 3 a.m. with your heart racing, skin itching, or your mind suddenly alert for no reason, it can feel scary — especially if it keeps happening. The good news? There are gentle, natural ways to calm a nighttime histamine dump and help your body settle back into rest.
These steps work because they support your nervous system, improve histamine breakdown, and help your gut rebalance while your body is trying to sleep.

Hydrate Slowly to Help Your Body Clear Histamine
Drinking a small amount of water — not chugging — can help your system process histamine more effectively.
Nighttime dehydration makes symptoms feel stronger, so a few sips can ease flushing, heart racing, and restlessness.
Try:
- A few sips of water
- Or a calming herbal tea like chamomile or ginger (if tolerated)
Use Gentle Deep Breathing to Settle Your Nervous System
Histamine activates your “fight-or-flight” system.
Slow breathing activates the opposite: your “rest-and-digest” system.
A simple method:
Inhale 4 seconds → Hold 1 → Exhale 6–8 seconds
Within 1–2 minutes, many people feel their heartbeat slow and muscles loosen.
Cool the Room Slightly to Reduce Histamine-Related Heat
Histamine widens blood vessels, which makes you feel hot or sweaty.
Lowering your room temperature by even 1–2 degrees can help calm that surge.
You can also try:
- Lifting the blanket off your feet
- Turning a fan toward the wall for indirect airflow
Small cooling signals reduce the body’s histamine response.
Avoid Checking Your Phone — Light Triggers More Histamine
Blue light suppresses melatonin (your sleep hormone) and increases alertness.
If you must use your phone, keep brightness low or turn on a red-light setting.
Even 10 seconds of bright light can fully wake your brain.
Try a Gentle Position Change
Sometimes histamine-related bloating or pressure makes lying down uncomfortable.
A slight position shift — like sleeping slightly propped up — can help ease:
- Chest tightness
- Heart racing
- Acid reflux
- Upper stomach pressure
Many people with histamine issues feel relief from a small incline.
Use Soothing, Low-Histamine Snacks if You Feel Weak
If your blood sugar dips at night, histamine symptoms feel more intense.
Safe options (only if truly needed):
- A banana
- A gluten-free rice cake
- A spoon of dairy-free yogurt
Avoid fermented foods — they’re high in histamine and can worsen symptoms.
Release Body Tension With a Quick “Reset” Stretch
Histamine activates nerves that tighten muscles.
A simple 20–30 second stretch can interrupt the cycle.
Try:
- Reaching both arms overhead
- Rolling your shoulders back
- Flexing and releasing your toes
This tricks your nervous system into shifting away from panic mode.
Remind Yourself: This Is a Histamine Surge — Not an Emergency
One of the most overlooked triggers is fear.
Histamine dumps mimic anxiety, so your brain interprets it as danger — and releases even more histamine.
Telling your mind what’s happening helps turn off the loop:
“This is just a histamine surge. It will pass.”
People underestimate how much this simple step helps.
Frequently Asked Questions
Can a nighttime histamine dump happen even if I eat low-histamine foods all day?
Yes. A histamine surge at night isn’t always about what you ate. Stress, hormones, poor sleep, dehydration, and mast-cell activation can trigger a release even when your diet is perfect. Many people with histamine sensitivity report nighttime flares even on a clean low-histamine meal plan.
Why do I get itchy skin only at night and not during the day?
At night your body naturally raises histamine levels as part of the circadian rhythm. Melatonin shifts, lower cortisol, warmer body temperature, and lying horizontally all make nerve endings more sensitive, which can turn mild daytime irritation into noticeable nighttime itching.
Can a histamine dump wake me from deep sleep without any digestive symptoms?
Absolutely. Histamine is also a neurotransmitter, so a surge can trigger wakefulness, a racing heartbeat, or sudden alertness — even without gut symptoms. Many people feel only neurological signs like restlessness, buzzing sensations, or anxiety.
Is it normal to feel wired but exhausted after a nighttime histamine spike?
Yes. Histamine activates your brain’s wake centers. When it spikes, you feel “tired but wired,” meaning mentally alert but physically drained. This combination is extremely common and can last into the next morning.
Can dehydration make nighttime histamine symptoms worse?
Dehydration concentrates histamine in tissues and reduces your body’s ability to clear it. Even mild dehydration can worsen flushing, heart pounding, and nighttime anxiety-like symptoms. Small sips of water often help.
Does sleeping in a warmer room increase the chance of a histamine dump?
Yes. A warm sleeping environment increases vasodilation (widening of blood vessels), which can amplify histamine’s effects. Many people notice fewer symptoms when sleeping slightly cooler with breathable bedding.
Can certain supplements make nighttime histamine spikes worse?
Some supplements — especially fermented ones, probiotics containing histamine-producing strains, magnesium glycinate, niacin, or aged herbal products — can raise histamine levels. If symptoms worsen after taking supplements at night, timing may be the issue.
Can I have a histamine dump even if my allergy tests come back normal?
Yes. Histamine intolerance and mast-cell hypersensitivity do not always show up on classic allergy testing. Many people with nighttime histamine dumps have perfectly normal IgE tests but still struggle with histamine clearance.
Does poor sleep itself increase nighttime histamine reactions?
Poor sleep raises inflammatory cytokines, lowers cortisol stability, and increases mast cell activity — all of which make nighttime histamine spikes more likely. A disrupted sleep schedule alone can trigger a flare even with a clean diet.
Can my menstrual cycle affect nighttime histamine symptoms?
Yes. Histamine and estrogen influence each other. During high-estrogen phases, histamine can spike more easily — especially at night when cortisol naturally dips. Many women report worse nighttime symptoms in mid-cycle or right before their period.
Conclusion
Handling histamine dump at night symptoms can be exhausting, especially when they wake you up suddenly and leave you foggy the next day. But once you understand why these nighttime spikes happen — stress, poor histamine breakdown, gut imbalance, or cortisol dips — the whole experience becomes less scary and more manageable.
Simple changes like lowering evening stress, choosing low-histamine dinners, supporting your gut, and improving your sleep routine can dramatically reduce nighttime reactions. And if symptoms keep happening, a provider can help uncover deeper issues like MCAS or gut dysbiosis.
You’re not imagining these night symptoms — and you’re not stuck with them. With the right habits and awareness, you can calm the reaction, sleep better, and feel more in control of your nights again.
References
- Maintz, L., & Novak, N. Histamine and histamine intolerance. The American Journal of Clinical Nutrition.
https://doi.org/10.1093/ajcn/85.5.1185 - Manzotti, G., Breda, D., et al. Food-induced histaminosis: Symptoms and treatment. Nutrients.
https://doi.org/10.3390/nu10111763 - Kovacova-Hlinkova, V., et al. Diamine oxidase and its role in histamine metabolism. International Journal of Molecular Sciences.
https://doi.org/10.3390/ijms20040872 - Gupta, P., & Patel, P. Histamine intolerance: The role of the gut. Frontiers in Immunology.
https://doi.org/10.3389/fimmu.2019.01384 - Rohleder, N. Stress and inflammation: The link and clinical implications. Psychoneuroendocrinology.
https://doi.org/10.1016/j.psyneuen.2014.03.012
(Discusses cortisol, immune activation, nighttime inflammatory spikes) - Pal, S., & Alam, R. Circadian rhythm of histamine secretion and sleep regulation. Sleep Medicine Reviews.
https://doi.org/10.1016/j.smrv.2019.101249 - Smolensky, M., Hermida, R., & Portaluppi, F. Circadian rhythms and nighttime physiological patterns. Chronobiology International.
https://doi.org/10.3109/07420520903420062
(Covers 24-hour rhythms, nighttime histamine-linked awakenings) - Theoharides, T. C., & Tsilioni, I. Mast cell activation and nighttime symptom flares. Journal of Allergy and Clinical Immunology.
https://doi.org/10.1016/j.jaci.2018.07.015 - Buckley, T. M., & Schatzberg, A. F. On the interactions of the HPA axis and sleep:
Journal of Psychiatric Research
https://doi.org/10.1016/j.jpsychires.2004.07.008
(Explains cortisol spikes at night → worsening inflammatory + histamine symptoms) - Irwin, M. R., & Opp, M. R. Sleep health and inflammation. Nature Reviews Immunology.
https://doi.org/10.1038/s41577-017-0001-9
(Links poor sleep with inflammatory pathways, mast cell activity, histamine)
