If you’ve recently been diagnosed with Hashimoto’s thyroiditis, you’re likely searching for ways to feel better day to day—especially when fatigue, brain fog, weight changes, or digestive issues start affecting your quality of life. While medication is often essential, many people with Hashimoto’s also explore dietary changes to support their overall well-being.
Research suggests that nutrition can influence inflammation, gut health, and nutrient status, all of which play a role in autoimmune conditions. That said, there is no single diet that works for everyone with Hashimoto’s, and responses to food can vary widely from person to person.
This guide takes a practical, food-first approach to eating with Hashimoto’s thyroiditis. Instead of promoting extreme restrictions or one-size-fits-all rules, it focuses on commonly studied dietary patterns, nutrient-dense foods, and lifestyle considerations that may help support thyroid health when used alongside medical care.
This content is for educational purposes only and is not a substitute for professional medical advice. Always work with a qualified healthcare provider when making changes to your diet or treatment plan.
Contents
- 1 Why Food Choices Matter in Hashimoto’s Thyroiditis
- 2 What Research Suggests About Diet and Hashimoto’s
- 3 Foods Commonly Included in a Hashimoto’s-Friendly Diet
- 4 Foods Some People with Hashimoto’s Choose to Limit
- 5 Sample 7-Day Meal Ideas for Hashimoto’s Thyroiditis
- 6 Lifestyle Habits That May Support Thyroid Health
- 7 Common Questions About Eating with Hashimoto’s
- 8 Final Thoughts on Supporting Thyroid Health Through Diet
- 9 References
Why Food Choices Matter in Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune condition where the body attacks its thyroid gland, often leading to hypothyroidism. While medication helps reset the thyroid gland and regulate hormone levels, diet can significantly influence how patients feel day to day. A well-thought-out Hashimoto Disease Diet Plan can help reduce symptoms, improve energy, and support immune health. Here’s why diet matters:
- Supports immune system balance – Anti-inflammatory foods can help calm the immune response and reduce flare-ups.
- Reduces systemic inflammation – Choosing the right diet for Hashimoto’s thyroiditis can lower chronic inflammation that worsens symptoms.
- Promotes gut health – A healthy gut is key in autoimmune conditions; avoiding trigger foods like gluten or processed sugars can improve digestion and reduce bloating.
- Improves nutrient absorption – Nutrient-dense foods ensure the body gets enough selenium, zinc, vitamin D, and other nutrients essential for thyroid function.
- Stabilizes energy and mood – A consistent, balanced Hashimoto’s diet helps regulate blood sugar levels, which supports energy, mood, and mental clarity.
- Supports thyroid hormone conversion – Certain foods can enhance the conversion of T4 to active T3, improving thyroid hormone effectiveness in the body.
What Research Suggests About Diet and Hashimoto’s
If you’re living with Hashimoto’s thyroiditis, you’ve probably noticed that food choices can affect how you feel—even if diet isn’t a cure. Research supports this idea in a practical way: while food alone can’t treat Hashimoto’s, it may influence inflammation, digestion, energy levels, and overall well-being.
Some studies have looked at gluten-free diets, especially in people who also have celiac disease or known gluten sensitivity. In those cases, removing gluten has been linked to improvements in digestive symptoms and, for some individuals, changes in thyroid antibody levels. For others, gluten doesn’t seem to make a noticeable difference, which is why a one-size-fits-all approach rarely works.
Many healthcare professionals encourage anti-inflammatory eating patterns for people with autoimmune conditions. Diets centered on vegetables, fruits, healthy fats, and minimally processed foods may help support immune balance and reduce inflammation over time—even if they don’t directly “fix” the thyroid.
Nutrients such as selenium, zinc, vitamin D, and iodine also play important roles in thyroid health. Research suggests that correcting deficiencies can be helpful, but more isn’t always better. Taking supplements without testing or guidance can sometimes do more harm than good, so personalization is key.
There’s also growing interest in the link between gut health and autoimmune conditions. Supporting digestion with fiber-rich foods and fermented foods, when tolerated, may help some people feel better by supporting a healthier gut environment.
Overall, current research points toward a flexible, personalized approach to diet. Paying attention to how your body responds and working alongside a healthcare provider is often more effective than following strict food rules.
Foods Commonly Included in a Hashimoto’s-Friendly Diet
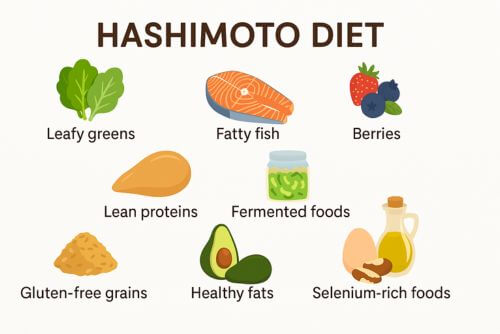
When creating a Hashimoto Disease Diet Plan, focusing on nutrient-rich, anti-inflammatory foods can help reduce symptoms and support thyroid and immune function. The right food choices can make a real difference in how you feel, especially when they support gut health, hormone balance, and overall wellness. Here are the key foods to include:
- Leafy greens and cruciferous vegetables (cooked) – Spinach, kale, and broccoli (in moderation and cooked) provide fiber, antioxidants, and vital nutrients like magnesium and vitamin A.
- Fatty fish and omega-3 sources – Salmon, sardines, chia seeds, and walnuts help fight inflammation and support brain and heart health.
- Lean proteins – Turkey, chicken, and grass-fed beef supply amino acids essential for muscle repair, energy, and immune support.
- Gluten-free whole grains – Quinoa, brown rice, and buckwheat are gentle on digestion and provide steady energy.
- Healthy fats – Avocados, olive oil, coconut oil, and flaxseeds support hormone production and reduce inflammation.
- Fruits rich in antioxidants – Berries, apples, and citrus fruits help neutralize free radicals and support immune function.
- Selenium-rich foods – Brazil nuts, eggs, and tuna contain selenium, which supports thyroid hormone conversion and immune health.
- Fermented foods and probiotics – Yogurt (if dairy-free), sauerkraut, kimchi, and kefir help balance gut bacteria and support digestion.
Foods Some People with Hashimoto’s Choose to Limit
When managing Hashimoto’s thyroiditis, many people find that certain foods can make symptoms like fatigue, bloating, joint pain, or brain fog worse. That doesn’t mean these foods are harmful for everyone—but paying attention to how your body responds can be an important part of feeling your best.
Here are some foods that people with Hashimoto’s commonly choose to limit or eliminate, especially during an elimination or healing phase.
Gluten-containing grains
Wheat, barley, and rye are often removed first, particularly by people with celiac disease or gluten sensitivity. Some research suggests gluten may contribute to immune activation in susceptible individuals, while others notice little difference. A trial period can help determine whether gluten affects you personally.
Dairy products
Milk, cheese, and other dairy foods may cause digestive discomfort or inflammation for some people with Hashimoto’s, especially those sensitive to lactose or casein. Others tolerate dairy well, so this is often an individual decision rather than a strict rule.
Highly processed foods and added sugars
Packaged foods high in refined sugars, additives, and preservatives may contribute to inflammation and blood sugar swings. Many people report feeling more stable and energized when they focus on whole, minimally processed foods instead.
Soy and soy-based products
Soy foods can interfere with thyroid hormone absorption when eaten in large amounts, particularly if consumed close to medication time. Some people choose to limit soy rather than eliminate it completely.
Industrial seed oils
Oils such as canola, corn, soybean, and sunflower oil are high in omega-6 fatty acids, which may promote inflammation when consumed in excess. Many people prefer olive oil, avocado oil, or coconut oil instead.
Nightshade vegetables (for some individuals)
Foods like tomatoes, eggplant, and peppers may aggravate joint pain or inflammation in certain people with autoimmune conditions, though many tolerate them without issue.
Artificial additives and preservatives
Some individuals notice symptom flare-ups when consuming foods with artificial colors, sweeteners, or preservatives. Reducing these can support gut health and overall immune balance.
The goal isn’t to create fear around food, but to identify what works best for your body. An elimination-and-reintroduction approach, ideally with guidance from a healthcare professional, can help you make informed choices without unnecessary restriction.
Sample 7-Day Meal Ideas for Hashimoto’s Thyroiditis

These meal ideas are meant to offer practical inspiration, not a strict or mandatory plan. People with Hashimoto’s often respond differently to foods, so flexibility is important. Use these examples as a starting point and adjust portions, ingredients, or meals based on your preferences, tolerances, and medical guidance.
All meals focus on whole, minimally processed foods, with an emphasis on balanced protein, healthy fats, fiber, and anti-inflammatory ingredients.
Day 1
- Breakfast: Scrambled eggs with spinach and sliced avocado
- Lunch: Grilled chicken salad with olive oil and lemon dressing
- Snack: Apple slices with almond butter
- Dinner: Baked salmon with quinoa and steamed broccoli
Day 2
- Breakfast: Chia seed pudding with coconut milk and blueberries
- Lunch: Turkey lettuce wraps with avocado and shredded carrots
- Snack: A handful of Brazil nuts
- Dinner: Stir-fried shrimp with bok choy and cauliflower rice
Day 3
- Breakfast: Smoothie with kale, banana, flaxseeds, and almond milk
- Lunch: Lentil soup with gluten-free toast (optional)
- Snack: Carrot sticks and hummus
- Dinner: Grilled chicken breast with roasted sweet potatoes and green beans
Day 4
- Breakfast: Gluten-free oatmeal topped with berries and chia seeds
- Lunch: Quinoa bowl with black beans, avocado, and roasted vegetables
- Snack: Hard-boiled egg and cucumber slices
- Dinner: Baked cod with wild rice and sautéed zucchini
Day 5
- Breakfast: Coconut yogurt with walnuts and raspberries
- Lunch: Tuna salad with mixed greens and pumpkin seeds
- Snack: Pear and a handful of sunflower seeds
- Dinner: Turkey meatballs with spaghetti squash and tomato basil sauce
Day 6
- Breakfast: Sweet potato hash with eggs and kale
- Lunch: Grilled veggie wrap in a gluten-free tortilla
- Snack: Smoothie with spinach, berries, and protein powder
- Dinner: Grilled lamb chops with mashed cauliflower and asparagus
Day 7
- Breakfast: Almond flour pancakes with maple syrup and a side of berries
- Lunch: Chicken and avocado salad with lemon tahini dressing
- Snack: Celery sticks with cashew butter
- Dinner: Stuffed bell peppers with ground turkey and brown rice
Lifestyle Habits That May Support Thyroid Health
While following a well-balanced Hashimoto’s Disease Diet Plan is essential, lifestyle choices also play a major role in managing symptoms and improving quality of life. When paired with the right nutrition, these supportive habits can enhance thyroid function, reduce flare-ups, and boost overall well-being:
- Prioritize quality sleep – Aim for 7–9 hours of consistent, restful sleep to support hormone balance and immune function. Poor sleep can worsen fatigue, brain fog, and inflammation.
- Manage stress levels – Chronic stress can trigger autoimmune activity. Practices like yoga, deep breathing, journaling, or gentle exercise can help calm the nervous system.
- Exercise mindfully – Low-impact activities like walking, swimming, or Pilates support energy and circulation without overtaxing the body. Avoid overtraining, which can worsen fatigue.
- Stay hydrated – Drinking enough water supports metabolism, digestion, and detoxification, key for those with thyroid issues.
- Avoid environmental toxins – Limit exposure to endocrine disruptors found in plastics, pesticides, and synthetic beauty products. Choose natural, non-toxic alternatives when possible.
- Support gut health – Incorporate fermented foods, probiotics, and prebiotic fiber to keep your gut microbiome balanced, which directly affects immune health.
- Regular lab testing and check-ins – Work with a healthcare provider to monitor thyroid levels, nutrient status, and adjust your diet or medication as needed.
Incorporating these lifestyle tips along with your Hashimoto’s thyroiditis diet can help you feel more in control, more energized, and better equipped to manage your symptoms long term.
Common Questions About Eating with Hashimoto’s
Can Hashimoto’s disease be managed through diet alone?
No, diet alone usually isn’t enough. While a proper Hashimoto’s Disease Diet Plan can help manage symptoms and reduce inflammation, most people still need thyroid hormone replacement prescribed by a doctor.
Is intermittent fasting safe for people with Hashimoto’s?
It can be, but it depends on the individual. Some with Hashimoto’s do well on gentle intermittent fasting, while others may feel fatigued or stressed. Always consult your doctor before starting.
Can dairy worsen Hashimoto’s symptoms?
Yes, for some people. Dairy can trigger inflammation or digestive issues in those with Hashimoto’s, especially if there’s a sensitivity. An elimination trial can help you find out.
Are there supplements that support a Hashimoto’s-friendly diet?
Yes. Selenium, zinc, vitamin D, and magnesium are often helpful, but it’s best to test your levels and talk with a healthcare provider before adding supplements.
Is a plant-based diet good for Hashimoto’s?
A well-planned plant-based diet can be helpful if it includes enough protein, iron, and key nutrients. However, some may need to limit goitrogenic foods like raw broccoli and kale.
Final Thoughts on Supporting Thyroid Health Through Diet
Living with Hashimoto’s thyroiditis often means learning how to work with your body, not against it. While diet alone can’t treat or cure the condition, thoughtful food choices may help support energy levels, digestion, and overall well-being when used alongside proper medical care.
The most helpful approach is usually a flexible, individualized one—focusing on whole, nutrient-dense foods, paying attention to how your body responds, and making adjustments as needed over time. What feels supportive for one person may not work the same way for another, and that’s completely normal with autoimmune conditions.
If you’re considering dietary changes, working with a qualified healthcare provider can help ensure your approach is both safe and appropriate for your needs. Use this guide as a starting point, stay curious about your body’s signals, and take changes one step at a time.
The information in this article is based on publicly available research and is intended for educational purposes only.
References
- Ruggeri RM, et al. (2018). Autoimmune thyroid disease and gluten-related disorders. Frontiers in Endocrinology.
- Krysiak R, et al. (2019). The effect of a gluten-free diet on thyroid autoimmunity in drug-naïve women with Hashimoto’s thyroiditis. Experimental and Clinical Endocrinology & Diabetes.
- Wichman J, et al. (2016). Selenium supplementation in autoimmune thyroiditis. Journal of Clinical Endocrinology & Metabolism.
- Rayman MP. (2012). Selenium and human health. The Lancet.
- Fasano A. (2020). All disease begins in the gut? Science Translational Medicine.
- Gao X, et al. (2021). Dietary patterns and inflammation. Advances in Nutrition.
