Living with PCOS can make weight loss feel confusing, exhausting, and unfair. Many women do “everything right” — eating less, exercising more — and still struggle to see changes on the scale. This isn’t a lack of willpower. It’s the result of how PCOS affects hormones, insulin, and metabolism.
A PCOS diet plan to lose weight isn’t about extreme restriction, cutting entire food groups, or following rigid meal rules. It’s about working with your hormones, stabilizing blood sugar, and choosing foods that support your body instead of fighting it. When meals are built around protein, fiber, healthy fats, and low-glycemic carbohydrates, many women notice improvements not only in weight, but also in energy levels, cravings, and cycle regularity.
In this guide, you’ll learn a realistic, science-informed approach to eating with PCOS. We’ll focus on practical strategies, flexible meal ideas, and sustainable habits that support weight loss while also addressing common PCOS symptoms like fatigue, insulin resistance, and abdominal weight gain. No extremes, no quick fixes — just a clear framework you can adapt to your own body and lifestyle.
Contents
- 1 What Is PCOS and Why Weight Loss Feels Different
- 2 Can PCOS Cause Weight Loss? What Weight Changes Really Mean
- 3 Download Free PDF
- 4 How Insulin Resistance Affects Weight in PCOS
- 5 What a PCOS Diet Plan to Lose Weight Should Focus On
- 6 Best Foods to Support Weight Loss With PCOS
- 7 Foods That May Slow Weight Loss With PCOS
- 8 Building Balanced Meals for PCOS Weight Loss
- 9 Sample PCOS-Friendly Meal Ideas (Flexible Examples)
- 10 Download Free PDF
- 11 Lifestyle Factors That Support Weight Loss With PCOS
- 12 How Long Does Weight Loss Take With PCOS?
- 13 When to Get Extra Support for PCOS Weight Management
- 14 Key Takeaways for Losing Weight With PCOS
- 15 References
What Is PCOS and Why Weight Loss Feels Different
If you have PCOS and feel like weight loss doesn’t work the way it “should,” you’re not imagining it — and it’s not a personal failure. Polycystic Ovary Syndrome affects how your hormones, metabolism, and blood sugar interact, which can make common weight-loss advice feel ineffective or even discouraging.
Understanding what’s happening inside your body helps explain why PCOS weight loss often requires a different approach — one that works with your hormones instead of against them.
How PCOS Changes Hormones and Metabolism
PCOS is a hormonal condition that affects ovulation, but its impact goes far beyond the reproductive system. Many women with PCOS have higher levels of androgens (often called male hormones), which can influence appetite, fat storage, and how the body uses energy.
At the same time, PCOS can alter metabolic signaling — meaning your body may not process glucose and calories as efficiently as someone without the condition. This hormonal-metabolic combination helps explain why weight gain can happen more easily and weight loss may feel slower.
Insulin Resistance and Weight Gain With PCOS
One of the most important factors in PCOS-related weight challenges is insulin resistance. Insulin is the hormone that moves sugar from your bloodstream into your cells for energy. When your cells don’t respond well to insulin, your body produces more of it.
Higher insulin levels promote fat storage, increase hunger signals, and make cravings harder to manage — even when you’re eating reasonably. This is why many women with PCOS struggle to lose weight despite cutting calories or exercising more.
Why PCOS Weight Often Collects Around the Abdomen
If you notice that weight tends to settle around your midsection, you’re not alone. Hormonal patterns common in PCOS — especially elevated insulin and androgens — are linked to increased abdominal fat storage.
This type of fat is more resistant to loss and more sensitive to stress hormones, which is why aggressive dieting or over-exercising can sometimes backfire instead of helping.
Why Traditional Weight Loss Advice Often Falls Short
Most weight loss advice assumes normal insulin sensitivity and stable hormonal signaling. With PCOS, those assumptions don’t always apply. Strict calorie restriction can increase fatigue, raise cortisol levels, and worsen blood sugar swings — all of which can make weight loss harder.
That’s why PCOS-friendly approaches tend to focus on blood sugar balance, adequate protein and fiber, sleep, and stress management, rather than extreme restriction.
The Big Picture
PCOS doesn’t mean weight loss is impossible — it means your body responds differently. When you understand these differences, it becomes easier to choose strategies that are realistic, sustainable, and supportive of both your weight and your overall health.
Can PCOS Cause Weight Loss? What Weight Changes Really Mean
PCOS is most often linked to weight gain or difficulty losing weight due to insulin resistance, hormonal imbalance, and metabolic changes. Because of this, unintentional weight loss is not considered a typical symptom of PCOS.
However, some women with PCOS do experience weight loss under specific circumstances. When this happens, it’s usually indirect—meaning PCOS creates the background hormonal environment, while other factors influence the actual weight change.
Why Weight Loss Is Less Common in PCOS
Most of the physiological mechanisms associated with PCOS tend to favor fat storage rather than fat loss. Insulin resistance plays a major role by increasing circulating insulin levels, which encourages the body to store energy—especially around the abdomen.
Hormonal imbalances, including elevated androgens, can also affect appetite, energy use, and fat distribution. In addition, research suggests that some women with PCOS may have a slightly lower resting metabolic rate, making spontaneous weight loss less likely.
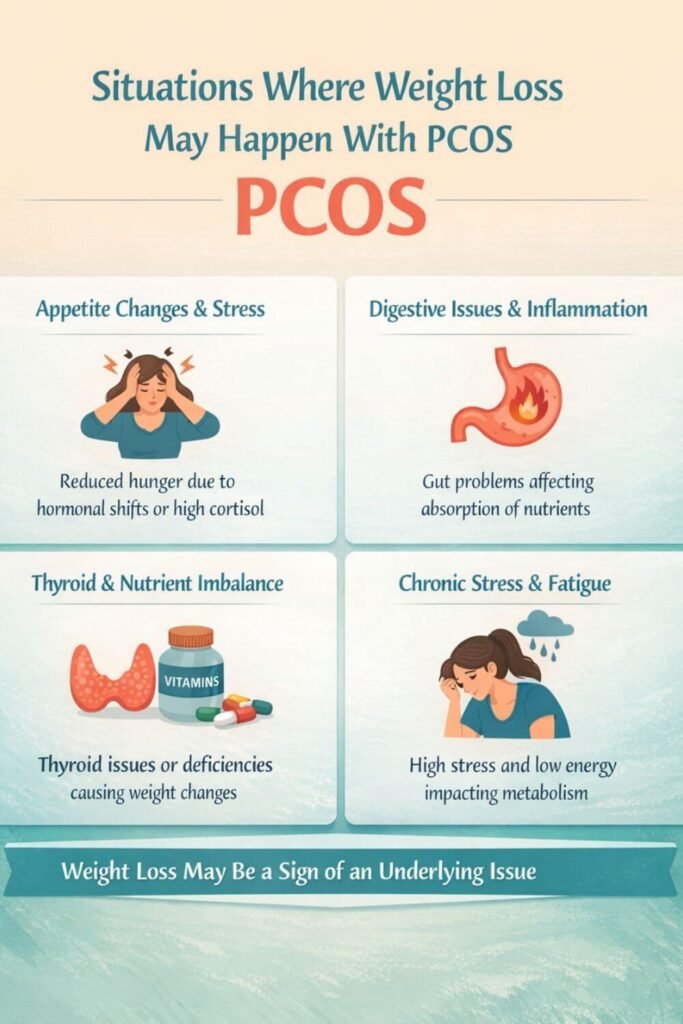
Situations Where Weight Loss Can Occur With PCOS
Although uncommon, weight loss may happen in women with PCOS when other factors come into play. These may include:
- Medication effects, such as reduced appetite from metformin or GLP-1 medications
- Stress and cortisol changes, which can temporarily suppress appetite or alter metabolism
- Thyroid imbalances, particularly hyperthyroidism, which can increase calorie burn
- Highly restrictive diets, which may cause short-term weight loss even in insulin-resistant states
In these situations, PCOS itself is usually not the direct cause of weight loss, but it can influence how the body responds to these triggers.
When Weight Loss With PCOS Deserves Medical Attention
Not all weight changes are harmful, but rapid or unexplained weight loss should not be ignored. Losing more than a small percentage of body weight without trying—especially if it happens quickly—may signal issues such as thyroid dysfunction, nutrient deficiencies, excessive stress, or digestive problems.
Pay attention if weight loss is accompanied by ongoing fatigue, worsening cycle irregularity, dizziness, hair thinning, or feeling generally unwell. In these cases, medical evaluation can help identify whether something beyond PCOS is contributing.
How Insulin Resistance Affects Weight in PCOS
If you have PCOS, you’ve probably heard the term insulin resistance — but understanding how it actually affects your weight can make a big difference in how you approach eating and lifestyle changes. Insulin resistance is one of the most common metabolic features of PCOS, and it plays a central role in why weight loss can feel so challenging.
What Insulin Resistance Means in PCOS
Insulin is a hormone that helps move glucose (sugar) from your bloodstream into your cells so it can be used for energy. With insulin resistance, your cells don’t respond efficiently to insulin, so your body produces more of it to keep blood sugar levels stable.
Many women with PCOS have some degree of insulin resistance — even those who are not overweight. This means weight struggles aren’t just about calories or willpower, but about how the body handles energy at a hormonal level.
How High Insulin Levels Promote Weight Gain
When insulin levels stay elevated, the body is more likely to store energy as fat rather than burn it. High insulin signals the body to:
- Store excess glucose as fat
- Slow down fat breakdown
- Increase hunger and cravings
This makes losing weight harder and explains why PCOS-related weight gain often happens even without major changes in food intake.
The Link Between Insulin and Abdominal Fat
Insulin resistance is strongly associated with increased fat storage around the abdomen. This type of fat is more metabolically active and more resistant to loss, which is why belly weight can feel especially stubborn with PCOS.
Abdominal fat also feeds back into insulin resistance, creating a cycle where weight gain and blood sugar imbalance reinforce each other unless addressed together.
Why Cutting Calories Alone Often Doesn’t Work
Traditional weight loss advice focuses on eating less, but with insulin resistance, severe calorie restriction can backfire. Eating too little may increase stress hormones, worsen blood sugar swings, and intensify cravings — making long-term weight loss harder to sustain.
This is why many women with PCOS respond better to strategies that stabilize blood sugar rather than simply reduce calories.
What This Means for Weight Loss With PCOS
Improving insulin sensitivity is often a key step in PCOS weight management. Approaches that emphasize balanced meals, adequate protein and fiber, regular movement, sleep, and stress reduction tend to support weight loss more effectively than extreme dieting.
When insulin resistance is addressed, weight loss often becomes more gradual — but also more sustainable and less exhausting.
What a PCOS Diet Plan to Lose Weight Should Focus On
When you’re living with PCOS, a diet plan for weight loss isn’t about eating as little as possible or following rigid rules. It’s about creating steady conditions in your body that support hormone balance, stable blood sugar, and sustainable energy. When those foundations are in place, weight loss becomes more achievable — and far less exhausting.
Blood Sugar Balance Comes First
One of the most important goals of a PCOS-friendly diet is keeping blood sugar levels stable throughout the day. Large spikes and crashes can worsen insulin resistance, increase cravings, and make fat loss harder.
Meals that combine protein, fiber, and healthy fats tend to digest more slowly and help prevent sharp blood sugar swings. This doesn’t mean eliminating carbohydrates completely — it means choosing carbohydrates that your body can handle more gently.
Adequate Protein at Every Meal
Protein plays a key role in PCOS weight management. It helps you feel full longer, supports lean muscle mass, and reduces the likelihood of overeating later in the day.
Including a reliable source of protein at each meal — whether from animal or plant-based options — can make a noticeable difference in appetite control and overall energy levels, especially for women dealing with insulin resistance.
Fiber-Rich Foods to Support Insulin Sensitivity
Fiber slows digestion and helps regulate how glucose enters the bloodstream. Diets higher in fiber are consistently associated with better insulin sensitivity, improved gut health, and easier weight control in women with PCOS.
Vegetables, legumes, seeds, and whole-food carbohydrate sources provide fiber while also delivering important micronutrients that support hormone function.
Healthy Fats for Hormone Support
Fats are often misunderstood in weight loss, but they’re essential for hormone production and satiety. Including moderate amounts of healthy fats can help meals feel satisfying and reduce the urge to snack excessively.
Sources like olive oil, nuts, seeds, avocados, and fatty fish support hormonal health without promoting blood sugar spikes when eaten in balanced portions.
Consistency Over Restriction
A PCOS diet plan works best when it’s consistent, not extreme. Highly restrictive eating patterns can raise stress hormones, disrupt cycles, and lead to rebound weight gain — even if short-term weight loss occurs.
Focusing on regular meals, realistic portions, and foods you can sustain long-term is far more effective than chasing rapid results.
Flexibility Based on Your Body’s Response
PCOS affects every woman differently. Some tolerate certain foods well, while others may notice symptoms like bloating, fatigue, or cravings after eating the same meals.
Paying attention to how your body responds — rather than following rigid food rules — allows you to adjust your diet in a way that supports both weight loss and overall well-being.
Best Foods to Support Weight Loss With PCOS
With PCOS, weight loss isn’t about finding a single “magic” food — it’s about choosing foods that help stabilize blood sugar, support hormone balance, and keep you feeling satisfied. The best foods for PCOS tend to work quietly in the background, reducing cravings and making healthy eating feel more manageable over time.
Protein-Rich Foods for Satiety and Metabolic Support
Protein is one of the most helpful nutrients for women with PCOS. It supports lean muscle mass, slows digestion, and helps prevent blood sugar spikes after meals.
Good protein choices include:
- Eggs
- Fish and seafood
- Poultry
- Lean meats
- Greek yogurt or skyr (if tolerated)
- Tofu and tempeh
Including protein at every meal can make a noticeable difference in appetite control and energy levels.
High-Fiber Vegetables for Blood Sugar Balance
Non-starchy vegetables are especially supportive for PCOS weight loss because they provide fiber with very little impact on blood sugar. Fiber helps slow glucose absorption and improves insulin sensitivity over time.
Vegetables like leafy greens, broccoli, zucchini, cauliflower, peppers, and asparagus can be eaten generously and paired easily with protein and healthy fats.
Low-Glycemic Carbohydrates That Support Energy
Carbohydrates don’t need to be eliminated for PCOS weight loss, but the type of carbohydrate matters. Low-glycemic carbs digest more slowly and are less likely to trigger insulin spikes.
Examples include:
- Beans and lentils
- Quinoa and oats (in moderate portions)
- Sweet potatoes
- Berries and whole fruits
These foods provide energy, fiber, and nutrients without the sharp blood sugar swings associated with refined carbs.
Healthy Fats That Support Hormones and Fullness
Healthy fats play an important role in hormone production and meal satisfaction. When included in balanced portions, they can help reduce overeating and improve meal adherence.
PCOS-friendly fat sources include:
- Olive oil
- Avocados
- Nuts and seeds
- Fatty fish like salmon and sardines
Pairing fats with fiber and protein helps keep blood sugar steady.
Anti-Inflammatory Foods for Hormonal Health
Low-grade inflammation is common in PCOS and may contribute to insulin resistance and metabolic stress. Choosing anti-inflammatory foods can support overall hormone balance.
These include:
- Fatty fish
- Berries
- Leafy greens
- Herbs and spices like turmeric and cinnamon
While no food “cures” PCOS, dietary patterns that reduce inflammation often support better metabolic outcomes.
The Takeaway
The best foods for PCOS weight loss are those that help your body feel stable, nourished, and satisfied. When meals consistently include protein, fiber, healthy fats, and low-glycemic carbohydrates, weight loss tends to become more gradual — and much more sustainable.
Foods That May Slow Weight Loss With PCOS
With PCOS, weight loss isn’t just about what you eat — it’s also about how certain foods affect your hormones and blood sugar. Some foods can make insulin resistance and cravings harder to manage, which may slow progress over time. This doesn’t mean these foods are “bad,” but being mindful of them can make weight loss feel more achievable.
Refined Carbohydrates and Added Sugars
Foods made with refined grains and added sugars tend to digest quickly and cause sharp blood sugar spikes. For women with PCOS, this can worsen insulin resistance and increase hunger soon after eating.
Common examples include:
- White bread, pastries, and baked goods
- Sugary cereals
- Candy and sweetened snacks
- Sugary drinks and fruit juices
These foods are often easiest to overeat and least satisfying, especially when eaten alone.
Highly Processed and Packaged Foods
Ultra-processed foods are typically high in refined carbohydrates, unhealthy fats, and additives that offer little nutritional value. They may contribute to inflammation and make appetite regulation more difficult.
This category includes:
- Fast food
- Packaged snack foods
- Frozen meals with long ingredient lists
- Processed meats
Eating these foods occasionally won’t derail progress, but relying on them regularly can make PCOS weight management more challenging.
Large Portions of High-Glycemic Carbohydrates
Carbohydrates aren’t the enemy in PCOS, but large portions of high-glycemic carbs can trigger insulin spikes when not balanced with protein or fat.
Examples include:
- White rice
- Regular pasta
- Potatoes prepared without protein or fiber
Portion size and food pairing matter more than complete avoidance.
Sugary Beverages and Liquid Calories
Drinks with added sugar or minimal fiber can raise blood sugar quickly without providing lasting fullness. This makes it easier to consume excess calories without feeling satisfied.
These include:
- Sweetened coffee drinks
- Sodas
- Energy drinks
- Sweetened teas
Choosing water, unsweetened tea, or coffee with minimal sweeteners can help stabilize energy levels.
Extremely Restrictive or “All-or-Nothing” Eating Patterns
Highly restrictive diets can increase stress hormones like cortisol and may worsen fatigue, cravings, and cycle irregularity. While short-term weight loss might happen, it often isn’t sustainable — especially with PCOS.
A balanced, flexible approach is more likely to support long-term weight loss and hormonal health.
The Takeaway
For PCOS, weight loss tends to slow when foods regularly trigger blood sugar swings, inflammation, or excessive restriction. Focusing on balance rather than perfection allows you to make progress without feeling deprived or overwhelmed.
Building Balanced Meals for PCOS Weight Loss
When you’re managing PCOS, weight loss doesn’t come from eating less at every meal — it comes from eating balanced meals that keep blood sugar steady and hormones supported. A balanced plate helps reduce cravings, improves energy, and makes weight loss feel far more sustainable over time.
Instead of strict rules, think in terms of structure and flexibility.
Start With a Solid Protein Base
Protein is the anchor of a PCOS-friendly meal. It slows digestion, supports muscle mass, and helps prevent the blood sugar spikes that can trigger hunger and cravings.
Aim to include a clear protein source at each meal, such as eggs, fish, poultry, lean meat, yogurt, tofu, or legumes. Even modest increases in protein can improve satiety and make portion control feel more natural.
Add Fiber-Rich Vegetables for Blood Sugar Control
Non-starchy vegetables add volume, fiber, and micronutrients without overwhelming blood sugar. They help meals feel filling while supporting insulin sensitivity.
Try to fill a generous portion of your plate with vegetables like leafy greens, broccoli, zucchini, cauliflower, peppers, or cucumbers. Variety matters — different colors provide different nutrients that support metabolic and hormonal health.
Include Carbohydrates Thoughtfully, Not Fearfully
Carbohydrates don’t need to be eliminated for PCOS weight loss, but they work best when eaten in appropriate portions and paired with protein and fat.
Choosing whole, low-glycemic carbohydrates — such as beans, lentils, oats, quinoa, or sweet potatoes — can support energy levels without triggering large blood sugar swings. Paying attention to portion size often matters more than cutting carbs entirely.
Use Healthy Fats to Improve Satisfaction
Healthy fats help meals feel satisfying and support hormone production. When included in balanced amounts, they can reduce the urge to snack and make meals more enjoyable.
Sources like olive oil, avocados, nuts, seeds, and fatty fish work well alongside protein and fiber-rich foods. A little goes a long way.
Keep Meals Regular and Predictable
Skipping meals or eating very irregularly can worsen blood sugar instability and increase cravings later in the day. Many women with PCOS find that eating consistent meals — rather than grazing or extreme fasting — supports better energy and appetite control.
Listening to hunger and fullness cues, rather than forcing strict schedules, can also help reduce stress around food.
The Takeaway
Building balanced meals for PCOS weight loss is about creating steady conditions for your body to function well. When meals consistently include protein, fiber, healthy fats, and thoughtfully chosen carbohydrates, weight loss becomes more manageable — and far less exhausting.
Sample PCOS-Friendly Meal Ideas (Flexible Examples)
These meal ideas are meant to give you inspiration — not rules. With PCOS, what works best can vary from person to person, so think of these as flexible combinations you can adapt based on your preferences, hunger levels, and how your body responds.
The common thread in all of them is balance: protein, fiber, healthy fats, and steady energy.
PCOS-Friendly Breakfast Ideas
Many women with PCOS feel better starting the day with protein to help stabilize blood sugar and reduce cravings later on.
Examples include:
- Eggs with sautéed vegetables and olive oil
- Greek yogurt with berries, seeds, and nuts
- Oatmeal paired with protein like eggs or yogurt
- Smoothies made with protein, fiber-rich fruits, and healthy fats
If you’re not hungry first thing in the morning, a lighter protein-focused option may work better than skipping entirely.
Balanced Lunch Ideas for PCOS
Lunches that combine protein and fiber tend to support steady energy through the afternoon.
Examples include:
- Grilled chicken or fish with a large salad and olive oil dressing
- Lentils or beans with vegetables and healthy fats
- Leftover protein and vegetables from dinner
- Tuna or egg salad served over greens rather than refined bread
Aim for meals that leave you comfortably full, not overly stuffed or still hungry.
PCOS-Friendly Dinner Ideas
Dinner doesn’t need to be overly light or restrictive. Balanced meals help prevent late-night cravings.
Examples include:
- Baked salmon with roasted vegetables
- Lean meat or tofu with stir-fried vegetables and a small portion of whole grains
- Vegetable-based dishes paired with a solid protein source
- Soups or stews made with beans, vegetables, and protein
Eating earlier in the evening and keeping meals balanced may support better sleep and digestion.
Snack Ideas That Support Blood Sugar Balance
Not everyone needs snacks, but when hunger strikes, pairing protein or fat with fiber can help prevent blood sugar crashes.
Examples include:
- Nuts with fruit
- Yogurt with seeds
- Vegetables with hummus
- Cheese with whole-food carbohydrates
Snacks should support your energy, not feel like a constant requirement.
The Takeaway
PCOS-friendly meals don’t have to be complicated or perfect. When you focus on balanced combinations and listen to your body’s cues, eating becomes less stressful — and weight loss feels more sustainable over time.
Lifestyle Factors That Support Weight Loss With PCOS
Food matters with PCOS — but it’s only part of the picture. Hormones, stress, sleep, and movement all influence how your body responds to a diet plan. When lifestyle factors are out of balance, even the “right” foods may not lead to weight loss.
Small, realistic changes in daily habits often make a bigger difference than extreme efforts.
Prioritizing Sleep for Hormone Balance
Sleep plays a major role in regulating insulin, appetite hormones, and stress levels. Poor or inconsistent sleep can increase insulin resistance and raise hunger hormones, making weight loss harder.
Many women with PCOS notice stronger cravings and lower energy after short or disrupted sleep. Aiming for consistent bedtimes, limiting screens before bed, and getting enough rest supports both metabolic health and weight regulation.
Managing Stress to Reduce Cortisol
Chronic stress raises cortisol, a hormone that can promote fat storage — especially around the abdomen. With PCOS, the body may be more sensitive to cortisol’s effects, which is why stress management is not optional, but essential.
Gentle practices like walking, breathing exercises, journaling, stretching, or short mindfulness sessions can help lower stress without adding more pressure to your routine.
Choosing the Right Type of Movement
Exercise supports insulin sensitivity and overall health, but more is not always better with PCOS. Excessive high-intensity workouts can increase stress hormones and worsen fatigue for some women.
Many find better results with a mix of:
- Strength training to support muscle and metabolism
- Low- to moderate-intensity cardio like walking or cycling
- Rest and recovery days
Consistency matters more than intensity.
Supporting Blood Sugar Throughout the Day
Lifestyle habits outside of meals also affect blood sugar stability. Long gaps without eating, skipping meals, or relying heavily on caffeine can increase blood sugar swings and cravings later.
Regular meals, hydration, and balanced snacks (when needed) help keep energy levels steady and reduce overeating.
Being Patient With Progress
PCOS-related weight loss is often slower — and that’s normal. Hormonal improvements typically come before visible changes on the scale. Many women notice better energy, fewer cravings, or improved cycles before weight shifts.
Focusing on trends over time rather than daily fluctuations helps reduce frustration and supports long-term success.
The Takeaway
Lifestyle factors quietly shape how your body responds to a PCOS diet plan. When sleep, stress, movement, and daily routines support hormone balance, weight loss becomes more sustainable — and far less exhausting.
How Long Does Weight Loss Take With PCOS?
If you’re doing “all the right things” and the scale isn’t moving as quickly as you hoped, you’re not alone. With PCOS, weight loss often follows a different timeline — and slower progress doesn’t mean your efforts aren’t working.
Understanding what a realistic timeline looks like can help reduce frustration and keep you consistent.
Why PCOS Weight Loss Is Often Slower
PCOS affects insulin sensitivity, hormones, and metabolism, all of which influence how efficiently the body burns fat. Even small improvements in blood sugar balance or hormone regulation can take time to translate into visible weight changes.
Many women experience internal improvements — like fewer cravings, better energy, or more regular cycles — before noticeable weight loss occurs.
What a Realistic Rate of Weight Loss Looks Like
For many women with PCOS, gradual weight loss is both safer and more sustainable. Losing even a small percentage of body weight over time can lead to meaningful improvements in insulin resistance and hormonal balance.
Rather than focusing on rapid changes, paying attention to steady trends over several weeks or months provides a more accurate picture of progress.
Why Non-Scale Wins Matter
With PCOS, progress doesn’t always show up first on the scale. Improvements in:
- Energy levels
- Appetite control
- Bloating
- Cycle regularity
- Cravings
often signal that your body is responding positively, even if weight loss is slow.
Tracking these changes can help you stay motivated and recognize success beyond the number on the scale.
When to Adjust Your Approach
If nothing changes after several weeks of consistent effort, it may be time to adjust your strategy — not abandon it. Small shifts in meal balance, sleep quality, stress management, or movement type can make a difference.
Support from a healthcare provider or registered dietitian familiar with PCOS can also help fine-tune your plan.
The Takeaway
Weight loss with PCOS takes patience. Progress often happens quietly at first, as hormones and blood sugar stabilize. When you give your body time to adapt and focus on sustainable habits, results tend to follow — even if they don’t happen overnight.
When to Get Extra Support for PCOS Weight Management
Trying to manage weight with PCOS can feel overwhelming at times, especially when progress is slow or inconsistent. Seeking extra support isn’t a sign of failure — it’s often a smart step toward finding an approach that works better for your body.
There are certain situations where professional guidance can make weight management safer, easier, and more effective.
If Weight Isn’t Changing Despite Consistent Effort
If you’ve been following balanced eating habits, supporting blood sugar, and maintaining healthy routines for several weeks or months without seeing changes, it may be time for additional support.
A healthcare provider or dietitian familiar with PCOS can help identify factors like insulin resistance severity, nutrient gaps, or lifestyle stressors that may be slowing progress.
If Symptoms Are Worsening or New Ones Appear
Weight management shouldn’t come at the cost of your overall well-being. If you notice worsening fatigue, irregular periods, hair loss, mood changes, or digestive issues, it’s important to check in with a professional.
These symptoms may signal hormonal shifts, thyroid issues, or nutritional imbalances that need attention beyond diet alone.
If You’re Considering Medication or Supplements
Some women with PCOS benefit from medications or targeted supplements to support insulin sensitivity or hormone balance. These options should always be discussed with a qualified healthcare provider.
Professional guidance helps ensure that any treatment supports weight management safely and fits into a long-term plan rather than offering short-term results only.
If Food Feels Stressful or Restrictive
If managing your diet feels emotionally exhausting, overly restrictive, or anxiety-provoking, extra support can be especially valuable. A registered dietitian can help you build a sustainable approach that supports both physical and mental health.
Long-term success with PCOS weight management depends on habits you can maintain without constant stress.
The Takeaway
PCOS weight management is not something you have to navigate alone. Getting extra support at the right time can help you uncover hidden barriers, protect your health, and move forward with more confidence and clarity.
Key Takeaways for Losing Weight With PCOS
Managing weight with PCOS can feel challenging, but understanding how your body works makes a real difference. Weight loss isn’t about perfection or extreme rules — it’s about building habits that support your hormones, metabolism, and long-term health.
Here are the most important points to keep in mind:
- PCOS changes how your body responds to food and exercise. Slower progress doesn’t mean you’re failing — it means your body needs a different approach.
- Blood sugar balance matters more than calorie cutting. Meals built around protein, fiber, healthy fats, and low-glycemic carbohydrates tend to support steadier energy and fewer cravings.
- Insulin resistance is a key factor. Supporting insulin sensitivity through diet, movement, sleep, and stress management often makes weight loss more achievable.
- Consistency beats restriction. Highly restrictive diets may lead to short-term changes but are harder to sustain and can backfire with PCOS.
- Lifestyle habits matter as much as food. Sleep, stress, and the type of movement you choose all influence hormones and weight regulation.
- Progress isn’t always visible on the scale first. Improvements in energy, appetite control, and cycle regularity often come before weight changes.
- Support is a strength, not a weakness. Working with a healthcare provider or dietitian familiar with PCOS can help you personalize your approach and avoid unnecessary frustration.
References
- Legro, R. S., Arslanian, S. A., Ehrmann, D. A., Hoeger, K. M., Murad, M. H., Pasquali, R., & Welt, C. K. (2013).
Diagnosis and treatment of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 98(12), 4565–4592.
https://doi.org/10.1210/jc.2013-2350 - Dunaif, A. (1997).
Insulin resistance and the polycystic ovary syndrome: Mechanism and implications for pathogenesis. Endocrine Reviews, 18(6), 774–800.
https://doi.org/10.1210/edrv.18.6.0318 - Moran, L. J., Pasquali, R., Teede, H. J., Hoeger, K. M., & Norman, R. J. (2009).
Treatment of obesity in polycystic ovary syndrome: A position statement of the Androgen Excess and Polycystic Ovary Syndrome Society. Fertility and Sterility, 92(6), 1966–1982.
https://doi.org/10.1016/j.fertnstert.2008.09.018 - Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., Piltonen, T., & Norman, R. J. (2018).
International evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(9), 1602–1618.
https://doi.org/10.1093/humrep/dey256 - Barber, T. M., Hanson, P., Weickert, M. O., & Franks, S. (2019).
Obesity and polycystic ovary syndrome: Implications for pathogenesis and novel management strategies. Clinical Medicine Insights: Reproductive Health, 13, 1–11.
https://doi.org/10.1177/1179558119874042
