If you have PCOS, you may have noticed changes in your body that don’t quite match your eating habits or activity level—especially around your abdomen. Many women describe feeling confused or frustrated by a belly that seems more prominent, bloated, or resistant to change. This often leads to a very common question: what does a PCOS belly actually look like?
A PCOS belly isn’t just about weight gain. It’s influenced by hormones, insulin resistance, and how the body stores fat, which means it can look and feel different from typical belly fat. Some women experience it even without being overweight, while others notice changes that appear suddenly or fluctuate throughout the day.
In this article, we’ll walk through the common physical signs of a PCOS belly, how it may differ from regular abdominal fat, and why these changes happen—using clear, medically responsible explanations. The goal is to help you better understand your body, without blame or fear, and with the reassurance that you’re not alone in this experience.
Contents
- 1 What Does a PCOS Belly Look Like?
- 2 Common Physical Signs of a PCOS Belly
- 3 PCOS Belly vs Normal Belly: What’s the Difference?
- 4 Can You Have a PCOS Belly Without Being Overweight?
- 5 Why PCOS Causes Fat to Collect Around the Abdomen
- 6 Symptoms That Often Appear Alongside a PCOS Belly
- 7 When to Talk to a Doctor
- 8 Final Thoughts
- 9 References
What Does a PCOS Belly Look Like?
If you have PCOS, the way your belly looks may feel confusing or even unfair—especially if your lifestyle hasn’t changed much. A PCOS belly doesn’t look the same for everyone, but there are common patterns many women notice. These changes are driven by hormones and insulin resistance, not a lack of effort or self-control.
Understanding these physical signs can help you recognize what’s happening in your body without jumping to conclusions or self-blame.
Fat Concentrated Around the Lower Abdomen
One of the most common signs of a PCOS belly is fat that settles primarily in the lower abdominal area, below the navel. This can happen even when the rest of the body remains relatively unchanged.
Many women describe:
- A lower belly that feels harder to lose
- Weight that appears “central” rather than evenly distributed
- A shape that becomes more noticeable in fitted clothing
This pattern is linked to how PCOS affects insulin and androgen levels, which influence fat storage.
A Bloated or Distended Appearance
A PCOS belly may also look bloated or swollen, especially after meals or at certain times of the month. This bloating can fluctuate from day to day, making the abdomen appear larger at some moments and smaller at others.
You might notice:
- Tightness or pressure in the abdomen
- Increased bloating after eating
- A belly that feels uncomfortable rather than just soft
This doesn’t always mean fat gain—it can be related to digestion, hormones, and fluid retention.
Disproportion Compared to the Rest of the Body
Another common experience is that the belly appears out of proportion compared to the hips, legs, or arms. Some women with PCOS feel that their midsection changes even when their overall weight stays stable.
This disproportion can be confusing and emotionally difficult, especially when:
- Weight gain feels sudden
- The belly changes without clear explanation
- Traditional weight-loss advice doesn’t seem to apply
These patterns are consistent with the way PCOS alters fat distribution.
Changes That May Appear Gradually or Suddenly
For some women, PCOS belly changes happen slowly over time. For others, they can feel sudden—especially during periods of hormonal shifts, increased stress, or changes in insulin sensitivity.
It’s also common for the belly to:
- Change throughout the menstrual cycle
- Look different at different times of day
- Become more noticeable during periods of fatigue or stress
These fluctuations are a normal part of how PCOS affects the body.
Common Physical Signs of a PCOS Belly
If you have PCOS, changes in your belly may feel subtle at first—or they may feel sudden and confusing. While not every woman with PCOS will notice the same physical signs, there are common patterns many women report. These signs are related to hormonal and metabolic factors, not personal habits or effort.
Recognizing these signs can help you better understand what your body may be experiencing.
Fat Concentrated Around the Lower Abdomen
One of the most frequently reported signs is fat that gathers mainly in the lower abdominal area. This can occur even if weight gain elsewhere is minimal.
You may notice:
- A lower belly that feels resistant to change
- Fat that appears more central rather than evenly spread
- A midsection that looks different from the rest of your body
This pattern is linked to how PCOS affects insulin and androgen levels.
A Belly That Appears Bloated or Distended
A PCOS belly may look bloated or swollen, especially after eating or during certain phases of the menstrual cycle.
Common experiences include:
- A tight or uncomfortable feeling in the abdomen
- Visible bloating that fluctuates throughout the day
- A belly that looks larger in the evening than in the morning
This bloating isn’t always caused by fat—it can also be influenced by digestion, fluid retention, and hormonal shifts.
A Firmer Feel Around the Abdomen
Some women describe their belly as feeling firmer or denser, rather than soft.
This may be related to:
- Visceral fat stored deeper in the abdomen
- Increased inflammation
- Hormonal effects on fat tissue
A firmer abdominal area can be one reason PCOS belly fat feels more stubborn.
Disproportion Compared to Hips, Legs, or Arms
Another common sign is a visible imbalance between the belly and other parts of the body.
You might notice:
- Slimmer legs or arms with a fuller midsection
- Changes in waist definition
- Clothing fitting differently around the abdomen
This disproportion is often connected to PCOS-related fat distribution rather than overall weight gain.
Fluctuations Throughout the Month
PCOS belly changes don’t always stay consistent.
Many women notice:
- Increased abdominal fullness during certain times of the cycle
- Belly size changing with stress or fatigue
- More bloating during periods of hormonal imbalance
These fluctuations are common and can make the belly feel unpredictable.
PCOS Belly vs Normal Belly: What’s the Difference?
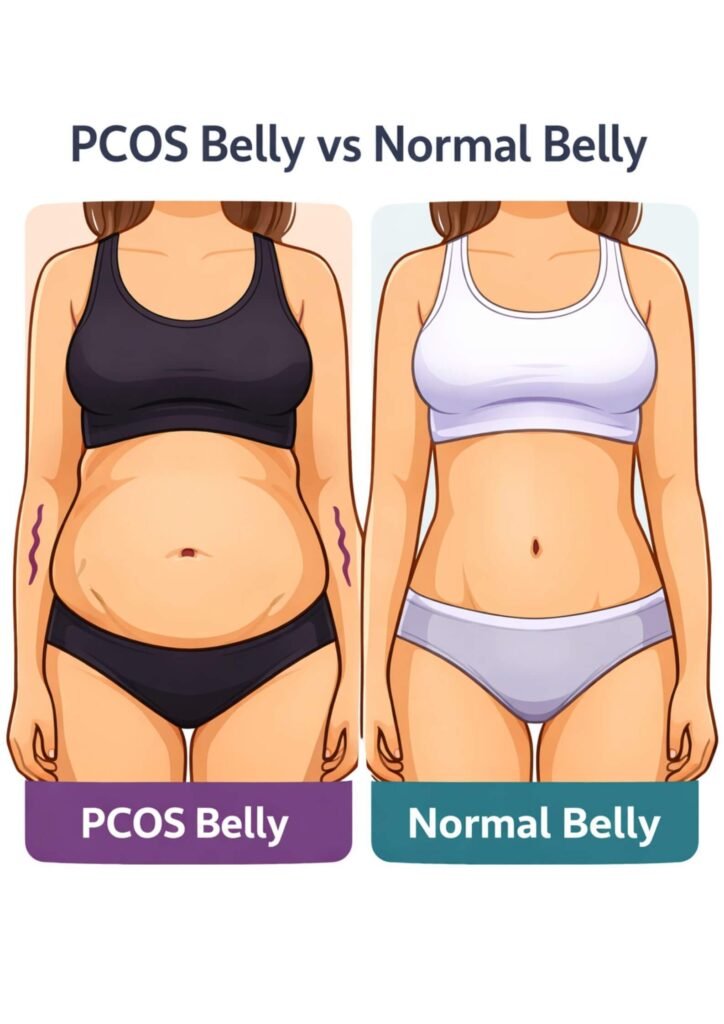
If you’re trying to understand whether the changes in your abdomen could be related to PCOS, comparing a PCOS-related belly to a typical belly shape can be helpful. The differences are not about appearance standards—they’re about how the body stores fat and responds to hormones.
It’s also important to remember that bodies naturally vary. These differences are patterns, not rules, and they don’t define your health or worth.
Fat Distribution Pattern
One of the main differences lies in where fat tends to collect.
- PCOS belly: Fat is more likely to be concentrated around the lower and central abdomen, even when weight gain elsewhere is minimal.
- Normal belly: Fat is usually distributed more evenly across the body, influenced mostly by genetics, age, and lifestyle.
This central pattern in PCOS is strongly influenced by hormonal signals rather than calorie intake alone.
Hormonal Influence
Hormones play a much larger role in a PCOS belly.
- PCOS belly: Often associated with insulin resistance and higher androgen levels, which encourage abdominal fat storage.
- Normal belly: Fat storage is less affected by hormonal disruption and more responsive to changes in diet and activity.
This is why PCOS belly fat can feel harder to change using traditional methods.
Fluctuation and Bloating
Another difference many women notice is how much the belly changes throughout the day.
- PCOS belly: May appear more bloated or swollen at certain times, especially after meals or during hormonal shifts.
- Normal belly: Usually changes less dramatically and feels more predictable day to day.
These fluctuations are often related to digestion, insulin response, and stress hormones.
Response to Lifestyle Changes
How the belly responds to lifestyle efforts can also differ.
- PCOS belly: May respond slowly and requires PCOS-specific approaches that support hormones and insulin sensitivity.
- Normal belly: Often responds more quickly to general diet and exercise changes.
This difference is one of the most frustrating aspects of PCOS—but it’s also an important clue that the body needs a different kind of support.
A Gentle Reminder
Having a PCOS belly does not mean something is “wrong” with your body. It means your body is responding to a hormonal condition that affects many women. Understanding these differences can help you move away from self-blame and toward strategies that actually make sense for you.
Can You Have a PCOS Belly Without Being Overweight?
Yes — it’s possible to have a PCOS-related belly even if you’re not overweight. This is one of the most confusing and frustrating aspects of PCOS for many women, especially when the rest of their body appears lean or unchanged.
PCOS affects the body in ways that go beyond overall weight, and belly changes are often linked to how fat is stored rather than how much fat there is.
Why Weight Alone Doesn’t Tell the Full Story
Body weight and Body Mass Index (BMI) don’t always reflect what’s happening metabolically.
With PCOS:
- Fat may be stored preferentially in the abdominal area
- Insulin resistance can be present at any weight
- Hormonal imbalance can affect fat distribution independently of BMI
This means someone can appear slim overall while still experiencing a fuller or more prominent abdomen.
The Role of Insulin Resistance at Normal Weight
Insulin resistance is common in PCOS and can occur even in women who are not overweight.
When insulin levels are elevated:
- The body is more likely to store fat in the abdomen
- Fat breakdown becomes less efficient in that area
- Abdominal fullness may persist despite stable weight
This helps explain why belly changes can occur without significant weight gain.
How Hormones Influence Fat Distribution
Hormonal shifts associated with PCOS—particularly higher androgen levels—can influence where fat is stored.
Rather than being evenly distributed:
- Fat may collect around the waist or lower abdomen
- Changes may appear gradually or fluctuate over time
- The belly may feel more noticeable compared to the rest of the body
These changes are driven by internal signals, not lifestyle failure.
Why This Experience Can Feel Invalidating
Many women feel dismissed when they seek answers because they don’t “look overweight.”
You may hear:
- “Your weight is normal, so everything is fine”
- “Just exercise more”
- “It’s probably bloating”
But your experience is real. PCOS doesn’t look the same on every body, and abdominal changes can be present even when weight appears healthy.
Why PCOS Causes Fat to Collect Around the Abdomen
If you have PCOS, you might wonder why fat seems to settle around your abdomen instead of being evenly distributed. This pattern isn’t random, and it’s not caused by lack of effort. PCOS affects how your body processes hormones and energy, which directly influences where fat is stored.
Understanding these underlying reasons can make the changes you see feel less confusing—and less personal.
Insulin Resistance and Abdominal Fat Storage
One of the most important factors is insulin resistance, which is common in PCOS.
When the body becomes less responsive to insulin:
- The pancreas produces more insulin to compensate
- Higher insulin levels signal the body to store fat
- Fat storage is more likely to occur around the abdomen
The abdominal area is especially sensitive to insulin, which is why PCOS-related fat often concentrates there rather than in other parts of the body.
Hormonal Imbalance and Androgen Levels
PCOS is often associated with elevated levels of androgens (sometimes called “male hormones”), which influence fat distribution.
Higher androgen levels can:
- Shift fat storage toward the abdomen
- Reduce fat storage in hips and thighs
- Make abdominal fat more persistent
This hormonal influence changes where fat is stored, not just how much fat the body carries.
Increased Visceral Fat Sensitivity
The abdomen contains a higher proportion of visceral fat, which is stored deeper around the organs.
Visceral fat:
- Is more hormonally active than subcutaneous fat
- Responds strongly to insulin and stress hormones
- Is more likely to accumulate when metabolic balance is disrupted
PCOS-related hormonal changes can increase the body’s tendency to store fat in this deeper abdominal area.
The Role of Stress Hormones
Stress hormones, particularly cortisol, also play a role.
In women with PCOS:
- Cortisol regulation may be more sensitive
- Chronic stress can worsen insulin resistance
- Elevated cortisol encourages abdominal fat storage
This helps explain why periods of stress, poor sleep, or overexertion can make abdominal changes more noticeable.
Why This Happens Even Without Major Weight Gain
Importantly, these mechanisms can occur without significant changes in overall body weight.
Because PCOS affects fat distribution rather than just fat quantity:
- Abdominal changes may appear first
- Weight may stay stable while shape changes
- The belly may become more prominent over time
This can feel confusing, but it reflects internal metabolic shifts rather than sudden weight gain.
A Compassionate Perspective
PCOS-related abdominal fat is not a personal failure or a reflection of poor habits. It’s the result of complex hormonal and metabolic interactions that many women experience.
Understanding why this happens can help shift the focus from frustration to informed self-care—and remind you that your body is responding to signals, not resisting your efforts.
Symptoms That Often Appear Alongside a PCOS Belly
A PCOS belly rarely appears in isolation. Many women notice other physical or internal changes happening at the same time, which can add to confusion or concern. These symptoms don’t mean something is suddenly “wrong,” but they often reflect the same hormonal and metabolic factors that influence abdominal fat distribution.
Not everyone with PCOS will experience all of these symptoms, and their presence or severity can vary widely.
Irregular or Unpredictable Menstrual Cycles
Changes in the menstrual cycle are one of the most common PCOS-related symptoms.
You may experience:
- Irregular periods
- Missed cycles
- Cycles that are longer or shorter than expected
Hormonal imbalance that affects ovulation can also influence how the body stores fat, particularly around the abdomen.
Increased Fatigue or Low Energy
Many women with PCOS report feeling unusually tired, even when they’re getting enough rest.
This fatigue may be linked to:
- Insulin resistance
- Blood sugar fluctuations
- Hormonal shifts
Low energy can make physical changes feel even more frustrating and harder to manage.
Increased Hair Growth or Hair Thinning
Changes in androgen levels can affect hair patterns.
Some women notice:
- Increased hair growth on the face, chest, or abdomen
- Thinning hair on the scalp
These symptoms and abdominal changes often share the same hormonal roots.
Acne or Oily Skin
Skin changes are another common companion symptom.
You might experience:
- Persistent acne beyond adolescence
- Oily skin that’s difficult to manage
These skin changes are often tied to androgen sensitivity, which can also influence fat distribution.
Digestive Discomfort or Bloating
Digestive symptoms frequently overlap with PCOS belly concerns.
Common experiences include:
- Bloating after meals
- Abdominal discomfort
- A feeling of fullness or pressure
These sensations can make the belly appear more prominent, even without changes in fat.
Mood Changes or Increased Stress Sensitivity
PCOS doesn’t only affect the body—it can affect emotional well-being too.
Some women report:
- Increased anxiety or irritability
- Mood fluctuations
- Feeling overwhelmed by physical changes
Stress hormones can interact with insulin and fat storage, making abdominal changes more noticeable during stressful periods.
A Helpful Reminder
Experiencing one or more of these symptoms alongside a PCOS belly doesn’t mean you should self-diagnose. Bodies are complex, and many conditions can share similar signs. However, noticing patterns can help you have more informed conversations with a healthcare provider if needed.
You’re not imagining these changes—and you’re not alone in noticing them.
When to Talk to a Doctor
Not every change in your belly or body means something is wrong. However, there are times when speaking with a healthcare provider can be helpful—especially if changes feel persistent, concerning, or are affecting your quality of life.
Seeking medical advice isn’t about overreacting; it’s about getting clarity and support when you need it.
If Abdominal Changes Appear Suddenly or Progress Quickly
If you notice your abdominal size or shape changing rapidly without a clear explanation, it’s reasonable to check in with a doctor.
Sudden changes may feel alarming, and a medical professional can help determine whether:
- Hormonal shifts are contributing
- Fluid retention or bloating is involved
- Other conditions should be ruled out
If Symptoms Begin to Interfere With Daily Life
When physical changes come with discomfort or emotional distress, support matters.
Consider speaking with a doctor if you experience:
- Ongoing abdominal pain or pressure
- Persistent bloating that doesn’t improve
- Fatigue that affects daily activities
- Anxiety or distress related to body changes
These experiences deserve attention, not dismissal.
If You Have Other PCOS-Related Symptoms
Abdominal changes combined with other PCOS-related symptoms may be a reason to seek guidance.
This can include:
- Irregular or absent periods
- Noticeable changes in hair growth or skin
- Difficulty managing energy levels
A healthcare provider can help assess whether these symptoms are connected and what steps, if any, are appropriate.
If You’re Unsure or Feeling Dismissed
You don’t need to have all the answers before talking to a doctor. If something doesn’t feel right—or if you feel your concerns haven’t been fully heard—it’s okay to ask more questions or seek a second opinion.
Your experiences are valid, even if test results appear “normal.”
Final Thoughts
Noticing changes in your belly can bring up a lot of questions, especially when you’re living with PCOS or suspect it may be affecting your body. A PCOS belly doesn’t look the same for everyone, and it isn’t a reflection of effort, discipline, or personal habits. It’s influenced by hormones, metabolism, and how your body responds internally.
Understanding what a PCOS belly can look like—and why it may differ from regular belly fat—can help replace confusion with clarity. This knowledge isn’t meant to label your body, but to help you recognize patterns and feel more informed when making health decisions.
If changes feel concerning or are accompanied by other symptoms, speaking with a healthcare provider can offer reassurance and guidance. And if nothing else, remember that you’re not alone in noticing these changes—many women with PCOS share similar experiences.
Your body is communicating, not failing. Listening with compassion is the first step toward understanding and care.
References
- Barber, T. M., Franks, S., McCarthy, M. I., & Wass, J. A. H. (2006). Metabolic characteristics of women with polycystic ovary syndrome. Clinical Endocrinology, 65(2), 137–145. https://doi.org/10.1111/j.1365-2265.2006.02572.x
- Dunaif, A. (1997). Insulin resistance and the polycystic ovary syndrome: Mechanism and implications for pathogenesis. Endocrine Reviews, 18(6), 774–800. https://doi.org/10.1210/edrv.18.6.0318
- Lim, S. S., Davies, M. J., Norman, R. J., & Moran, L. J. (2012). Overweight, obesity and central obesity in women with polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction Update, 18(6), 618–637. https://doi.org/10.1093/humupd/dms030
- Pasquali, R., Gambineri, A., & Pagotto, U. (2006). The impact of obesity on reproduction in women with polycystic ovary syndrome. BJOG: An International Journal of Obstetrics & Gynaecology, 113(10), 1148–1159. https://doi.org/10.1111/j.1471-0528.2006.00990.x
- Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., Piltonen, T., & Norman, R. J. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(9), 1602–1618. https://doi.org/10.1093/humrep/dey256
