Living with PCOS can feel frustrating, especially when symptoms like irregular periods, fatigue, acne, or weight changes start affecting daily life. If you’re searching for polycystic ovary syndrome treatment naturally, you’re likely looking for realistic ways to feel better—not quick fixes.
While PCOS isn’t considered permanently curable, research shows that lifestyle and dietary changes can help manage symptoms and support hormone balance over time. This article covers evidence-based, natural approaches—from nutrition and movement to stress and sleep—that you can adapt to your needs and discuss with your healthcare provider.
This content is for educational purposes only and not a substitute for medical advice.
Contents
- 1 Can Polycystic Ovary Syndrome Be Treated Naturally?
- 2 Natural Treatment Approaches That May Help Manage PCOS Symptoms
- 3 Best Diet Choices for Managing PCOS Naturally
- 3.1 Prioritize Meals That Stabilize Blood Sugar
- 3.2 Choose Carbohydrates That Support Insulin Sensitivity
- 3.3 Include Adequate Protein at Every Meal
- 3.4 Focus on Anti-Inflammatory Fats
- 3.5 Be Mindful With Dairy and Gluten (Individual Response Matters)
- 3.6 Support Gut Health Through Fiber and Variety
- 3.7 Avoid Extreme or Restrictive Dieting
- 3.8 The Goal: Consistency, Not Perfection
- 4 How Physical Activity Supports Hormone Balance in PCOS
- 5 Download Free PDF
- 6 Stress, Sleep, and Their Role in PCOS Hormone Regulation
- 6.1 Chronic Stress Can Feel Like Constant Fatigue and Mental Overload
- 6.2 High Cortisol Can Disrupt Your Cycle Without You Realizing Why
- 6.3 Poor Sleep Often Shows Up as Cravings, Low Energy, and Mood Swings
- 6.4 Sleep Disruption May Worsen Acne, Hair Growth, and Hormonal Symptoms
- 6.5 Irregular Sleep Patterns Can Make You Feel “Wired at Night, Tired in the Morning”
- 6.6 Stress Reduction Can Improve How You Feel Day to Day
- 6.7 Why This Matters for Natural PCOS Treatment
- 7 Supplements Commonly Used in Natural PCOS Treatment
- 8 Natural PCOS Treatment for Women Not Trying to Conceive
- 9 Can PCOS Go Away Permanently?
- 10 When to Seek Medical Treatment Alongside Natural Approaches
- 11 Frequently Asked Questions About Natural PCOS Treatment
- 11.1 How long does it usually take to see results from natural PCOS treatment?
- 11.2 Can PCOS symptoms come back after they improve?
- 11.3 Is natural PCOS treatment effective if I’m not overweight?
- 11.4 Can natural PCOS treatment help with acne or hair-related symptoms?
- 11.5 Do I need medical supervision when following natural PCOS treatment?
- 11.6 Is natural PCOS treatment a lifelong commitment?
- 12 Final Thoughts
- 13 References
- 14 Before Starting Hard Diets
- 15 Struggling with unsustainable diets and frustrated by the lack of results?
Can Polycystic Ovary Syndrome Be Treated Naturally?
If you’re considering natural options for PCOS, it helps to start with an honest expectation. PCOS isn’t considered permanently curable, but many people manage symptoms naturally and see meaningful long-term improvement.
Natural treatment focuses on supporting key factors linked to PCOS, including insulin resistance, inflammation, stress, and hormone balance. Research shows that addressing these areas can improve cycle regularity, energy levels, and overall well-being.
Natural Treatment Focuses on Management, Not a Cure
PCOS is a long-term condition, but symptoms can become more manageable over time. Lifestyle-based approaches have been shown to support metabolic and hormonal health when followed consistently.
Many people experience:
- More regular menstrual cycles
- Improved insulin sensitivity
- Reduced androgen-related symptoms
Consistency matters more than perfection.
Diet and Lifestyle Are the Foundation
Diet and lifestyle changes are considered first-line strategies in PCOS management. Balanced meals, regular movement, adequate sleep, and stress reduction help support insulin regulation and hormonal signaling.
These changes don’t need to be extreme — small, sustainable adjustments tend to work best long term.
Weight Loss Is Not Required
While weight loss can help some individuals, research shows that hormonal and metabolic improvements can occur without significant weight change. Natural PCOS treatment focuses on health markers, not the scale.
Natural Treatment Approaches That May Help Manage PCOS Symptoms
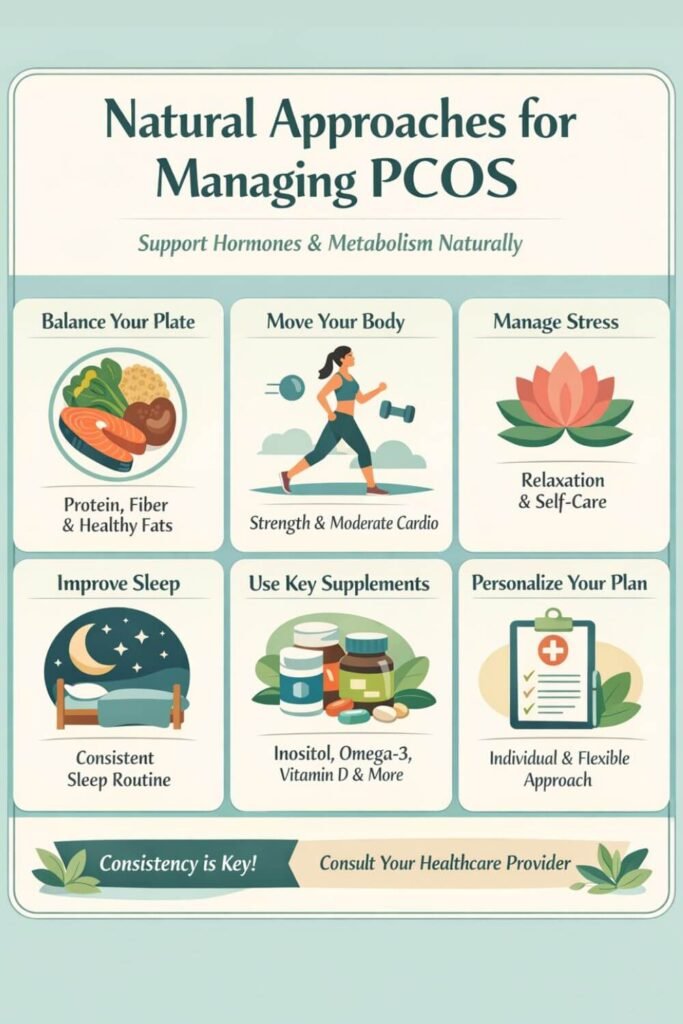
Managing PCOS naturally works best when you focus on a few core areas that influence hormones and metabolism, rather than trying to change everything at once. Clinical research consistently supports lifestyle-based strategies as meaningful tools for symptom management.
Core Natural Approaches That Support PCOS
Support insulin sensitivity
- Eat balanced meals with protein, fiber, and healthy fats
- Limit refined carbohydrates that cause blood sugar spikes
- Keep meal timing consistent
Improving insulin response supports hormone balance and cycle regularity.
Use nutrition to support hormone balance
- Prioritize whole grains, vegetables, legumes, and lean proteins
- Include anti-inflammatory fats like olive oil, nuts, and seeds
- Avoid overly restrictive dieting
The goal is steady energy and metabolic support, not perfection.
Move your body without overdoing it
- Choose moderate, consistent activity over extremes
- Combine strength training with low-impact cardio
- Avoid overtraining, which may increase stress hormones
Sustainable movement supports insulin sensitivity and hormone regulation.
Improve sleep quality
- Keep consistent sleep and wake times
- Limit late-night caffeine or heavy meals
- Create a calming nighttime routine
Better sleep supports insulin regulation, energy, and cycle stability.
Best Diet Choices for Managing PCOS Naturally
When it comes to PCOS, diet isn’t about restriction — it’s about supporting insulin sensitivity, hormone balance, and inflammation control. Research consistently shows that how you eat matters more than following any single named diet.
Below are the most evidence-supported dietary choices for managing PCOS naturally.
Prioritize Meals That Stabilize Blood Sugar
Blood sugar stability is one of the most important dietary goals in PCOS management. Frequent spikes and crashes can worsen insulin resistance and androgen imbalance.
What this looks like in practice:
- Pair protein + fiber + healthy fats at each meal
- Avoid eating carbohydrates alone
- Eat regular meals instead of skipping and overeating later
This approach helps reduce cravings, energy crashes, and hormonal stress.
Choose Carbohydrates That Support Insulin Sensitivity
PCOS doesn’t require eliminating carbohydrates, but carbohydrate quality matters.
Better choices include:
- Whole grains (oats, quinoa, brown rice)
- Legumes and beans
- Vegetables and lower-glycemic fruits
Limiting refined carbohydrates and added sugars can help improve insulin response over time, even without weight loss.
Include Adequate Protein at Every Meal
Protein supports blood sugar control, muscle mass, and appetite regulation — all important for PCOS.
Aim to include protein from:
- Eggs, fish, poultry, or lean meats
- Plant-based sources like lentils, tofu, or tempeh
- Greek yogurt or dairy-free alternatives, if tolerated
Consistent protein intake may help reduce cravings and support more stable cycles.
Focus on Anti-Inflammatory Fats
Chronic low-grade inflammation is commonly seen in PCOS. Certain fats help counter this process.
Prioritize:
- Olive oil and avocado
- Nuts and seeds
- Fatty fish rich in omega-3s
These fats support hormone production and may help improve metabolic markers linked to PCOS.
Be Mindful With Dairy and Gluten (Individual Response Matters)
Some people with PCOS notice symptom changes when reducing dairy or gluten, but research does not support universal elimination.
A short-term trial may be helpful if you experience:
- Digestive discomfort
- Worsened acne
- Increased bloating or inflammation
If no improvement is noticed, strict avoidance is usually unnecessary.
Support Gut Health Through Fiber and Variety
Emerging research links gut health to hormone regulation and insulin sensitivity.
Helpful habits include:
- Eating a variety of plant foods
- Including fiber-rich vegetables and legumes
- Avoiding highly processed foods that disrupt gut balance
Gut support is subtle but impactful over time.
Avoid Extreme or Restrictive Dieting
Very low-calorie diets, prolonged fasting, or highly restrictive eating patterns can increase stress hormones and worsen cycle irregularity in PCOS.
Sustainable, balanced eating consistently outperforms extremes when it comes to long-term symptom management.
The Goal: Consistency, Not Perfection
There is no single “perfect PCOS diet.” The most effective approach is one you can maintain long term, that supports steady energy, balanced hormones, and overall well-being.
Diet works best when combined with movement, stress management, and appropriate medical care.
How Physical Activity Supports Hormone Balance in PCOS
Physical activity plays a meaningful role in managing PCOS, not because it “burns calories,” but because of how it affects insulin sensitivity, androgen levels, stress hormones, and cycle regulation. The type, intensity, and consistency of movement matter more than doing as much as possible.
Exercise Improves Insulin Sensitivity
Insulin resistance is one of the most common underlying factors in PCOS, and physical activity is one of the most effective non-medical ways to improve it.
Research shows that regular movement helps:
- Increase glucose uptake by muscles
- Reduce circulating insulin levels
- Improve metabolic markers even without weight loss
This is why exercise benefits people with PCOS across different body sizes.
StrengStrength Training Supports Hormonal Stability
Strength and resistance training help improve insulin sensitivity by increasing muscle mass.
Key benefits include:
- Better blood sugar control
- Improved body composition
- Support for long-term metabolic health
Heavy lifting isn’t required—bodyweight exercises or light weights done consistently are enough.
Moderate Cardio Is Often More Sustainable
Low- to moderate-intensity cardio supports heart health without overstressing the body.
Good options include:
- Brisk walking
- Cycling
- Swimming
- Low-impact aerobics
These forms of movement are easier to maintain long-term and less likely to worsen fatigue or cycle irregularity.
High-Intensity Exercise Should Be Used Selectively
High-intensity workouts may help some people with PCOS, but too much can backfire.
Excessive intensity may:
- Raise cortisol
- Disrupt menstrual cycles
- Increase fatigue or inflammation
If workouts leave you feeling drained instead of energized, reducing intensity is often more supportive.
Movement Helps Regulate Stress Hormones
Enjoyable, low-stress movement can help regulate cortisol and support nervous system balance. Activities like walking, yoga, or gentle stretching often feel more restorative than exhausting.
Consistency Matters More Than Intensity
You don’t need a perfect workout plan. Research shows that regular, sustainable movement leads to better hormone regulation than sporadic intense exercise. Small amounts of movement, done consistently, add up over time.
Stress, Sleep, and Their Role in PCOS Hormone Regulation
If you have PCOS, stress and poor sleep often don’t show up as isolated issues — they show up as how you feel day to day. You might wake up already tired, feel wired but exhausted, crave sugar or caffeine by mid-morning, and feel emotionally overwhelmed by things that didn’t used to bother you.
These experiences aren’t imagined. Peer-reviewed research shows that stress and sleep directly influence the hormonal pathways involved in PCOS, especially cortisol, insulin, and androgens.
Chronic Stress Can Feel Like Constant Fatigue and Mental Overload
Living with PCOS often means feeling like your body is under pressure even when your life doesn’t look “that stressful” on the outside. You may notice:
- Feeling tired
- Brain fog
- Emotionally reactive
- Cravings
From a physiological perspective, chronic stress activates the HPA axis, increasing cortisol output. Research shows that elevated cortisol can worsen insulin resistance, which in turn stimulates ovarian androgen production — a key driver of PCOS symptoms.
This creates a cycle where stress feeds hormonal imbalance, and hormonal imbalance feeds more stress.
High Cortisol Can Disrupt Your Cycle Without You Realizing Why
You might notice your period becoming more irregular during stressful periods of your life, or ovulation seeming unpredictable. Studies suggest that elevated cortisol can interfere with the hypothalamic–pituitary–ovarian (HPO) axis, weakening the signals that regulate ovulation.
This can feel like:
- Cycles that suddenly lengthen or disappear
- Periods that don’t come when expected
- A sense that your body is “out of sync”
Stress doesn’t cause PCOS, but it can absolutely make symptoms harder to manage.
Poor Sleep Often Shows Up as Cravings, Low Energy, and Mood Swings
Many women with PCOS don’t just “sleep badly” — they wake up unrefreshed, feel drained during the day, and rely on caffeine to get through normal tasks.
Research shows that insufficient or fragmented sleep:
- Raises evening cortisol levels
- Alters appetite hormones like leptin and ghrelin
This hormonal shift can explain why you might feel hungrier, crave sugar or carbs more intensely, or feel emotionally low after poor sleep — even if your diet hasn’t changed.
Sleep Disruption May Worsen Acne, Hair Growth, and Hormonal Symptoms
Emerging evidence links poor sleep quality to higher androgen levels in women with PCOS. Elevated androgens are associated with acne, excess facial or body hair, scalp hair thinning, and cycle irregularity.
So if your skin flares or hair symptoms worsen during periods of poor sleep, there may be a hormonal explanation, not a lack of discipline or “doing something wrong.”
Irregular Sleep Patterns Can Make You Feel “Wired at Night, Tired in the Morning”
Hormones follow a circadian rhythm. Cortisol should be higher in the morning and gradually fall at night. When sleep timing is inconsistent, that rhythm can flatten.
This often feels like:
- Difficulty falling asleep despite exhaustion
- Feeling alert late at night
- Struggling to wake up in the morning
- Needing stimulants just to function
Research shows that disrupted circadian rhythm can worsen cortisol regulation, insulin sensitivity, and reproductive hormone signaling.
Stress Reduction Can Improve How You Feel Day to Day
Clinical studies show that reducing physiological stress — not just “thinking positively” — can improve metabolic and hormonal markers.
For many women with PCOS, stress reduction leads to:
- More stable energy levels
- Fewer cravings
- Improved emotional resilience
- Better tolerance to exercise and diet changes
This doesn’t require perfection. Gentle, consistent strategies are often enough to support hormone regulation.
Why This Matters for Natural PCOS Treatment
Natural PCOS treatment works best when your body isn’t constantly in survival mode. If stress and sleep are ignored, diet and exercise often feel harder than they need to be.
Supporting sleep and stress regulation helps create a hormonal environment where other treatments actually work, and where you feel more like yourself again.
Supplements Commonly Used in Natural PCOS Treatment
If supplements have ever felt confusing or overwhelming, you’re not alone. Many women with PCOS explore supplements because they’re looking for relief from fatigue, cravings, irregular cycles, acne, or feeling hormonally “out of sync.”
Supplements won’t treat PCOS on their own, but research shows some may support specific symptoms when used thoughtfully alongside lifestyle changes.
Inositols (Myo-Inositol and D-Chiro-Inositol)
Inositols are commonly used for blood sugar regulation and cycle irregularity. Studies suggest they may improve insulin sensitivity, support ovulation, and lower androgen levels in some women. Benefits tend to be gradual, not immediate.
Omega-3 Fatty Acids
Omega-3s are studied for their role in reducing inflammation and supporting metabolic health. Research shows modest benefits for lipid profiles and androgen-related markers, with many women reporting a more balanced overall feeling.
Vitamin D
Vitamin D deficiency is common in PCOS and linked to fatigue and metabolic challenges. When deficiency is corrected, some women notice improved energy, insulin response, and cycle regularity. Testing before supplementing is recommended.
Magnesium
Magnesium supports blood sugar control, sleep quality, and nervous system regulation. Research suggests it may help with sleep disturbances and stress-related symptoms, which often overlap with PCOS.
Zinc
Zinc is frequently discussed for acne and hair-related symptoms. Studies suggest it may support skin health and androgen metabolism, though changes are usually gradual.
N-Acetylcysteine (NAC)
NAC has been studied for insulin resistance and ovulatory function. Evidence suggests modest benefits, particularly in insulin-resistant PCOS, but it’s best viewed as supportive rather than corrective.
Supplements Aren’t About “Doing More”
It’s understandable to want something that makes PCOS feel easier to manage. But taking many supplements without a clear reason often leads to frustration.
The most helpful approach is:
- Targeted
- Personalized
- Used alongside nutrition, movement, sleep, and stress support
When supplements fit your needs, you may feel more supported — not pressured to fix yourself.
Natural PCOS Treatment for Women Not Trying to Conceive
If you’re not trying to conceive right now, managing PCOS can feel confusing. A lot of advice focuses heavily on fertility, even though your daily concerns may be more about energy, cycles, mood, weight changes, acne, or simply feeling balanced in your body.
Natural PCOS treatment doesn’t have to center on pregnancy. It can focus on long-term hormone and metabolic health, regardless of your reproductive goals.
Focus on Cycle Regulation and Hormone Balance
Even if pregnancy isn’t a priority, irregular or absent periods can still signal hormonal imbalance. Supporting cycle regularity helps protect long-term health, including metabolic and endometrial health.
Many women notice improvements through:
- Balanced, blood-sugar–supportive meals
- Consistent physical activity
- Stress and sleep support
The goal is rhythm and stability, not forcing a cycle.
Address Daily Symptoms That Affect Quality of Life
PCOS often shows up in everyday ways, not just lab results. You might deal with fatigue, cravings, brain fog, acne, or hair changes that affect confidence and well-being.
Natural strategies often focus on:
- Improving insulin sensitivity
- Reducing low-grade inflammation
- Supporting nervous system balance
Over time, many women feel steadier energy and fewer symptom flare-ups.
Prioritize Metabolic Health Now, Not Later
PCOS is associated with long-term metabolic risks, even in women who are not trying to conceive. Supporting insulin sensitivity and cardiovascular health early can make future management easier.
This includes:
- Sustainable nutrition habits
- Regular movement
- Avoiding extreme dieting or over-exercising
These habits support health now and in the future.
Medical Care Still Matters
Choosing natural treatment doesn’t mean avoiding medical care. Periodic check-ins, hormone monitoring, and professional guidance help ensure your approach remains safe and effective.
Natural and medical strategies often work best together, not in opposition.
PCOS Management Is About You — Not a Timeline
You don’t need to plan for pregnancy to deserve support for PCOS. Managing symptoms naturally can help you feel more in control, more comfortable in your body, and more confident in your health — wherever you are in life.
Can PCOS Go Away Permanently?
The honest answer is nuanced.
PCOS Is Not Considered Permanently Curable
Based on current medical understanding, PCOS is considered a chronic condition, meaning it doesn’t disappear completely. It’s influenced by genetics, hormone signaling, and metabolism — factors that don’t simply switch off.
That said, having PCOS doesn’t mean you’ll always feel unwell or symptomatic.
Symptoms Can Improve — Sometimes Dramatically
While PCOS itself doesn’t vanish, research and clinical experience show that symptoms can become mild or even unnoticeable for long periods of time.
Many women experience:
- More regular cycles
- Improved energy and mood
- Reduced acne or hair symptoms
- Better metabolic health
This often happens when underlying drivers like insulin resistance, inflammation, and chronic stress are well managed.
Why It Can Feel Like PCOS Has “Gone Away”
You may hear stories of women who say their PCOS “went away.” In most cases, what’s really happening is long-term symptom remission, not a permanent cure.
When hormones are better regulated and metabolic health improves, PCOS may no longer dominate daily life — which can feel like freedom after years of struggle.
Life Stages Can Change How PCOS Shows Up
PCOS symptoms don’t stay the same forever. They often shift with:
- Age
- Weight changes
- Stress levels
- Pregnancy or menopause
Some women notice symptoms lessen over time, while others see changes during major life transitions. This doesn’t mean PCOS is gone — it means it’s responsive to internal and external factors.
The Goal Is Long-Term Management, Not Erasing PCOS
Instead of aiming to “get rid of” PCOS, a more helpful goal is long-term management that supports how you want to feel.
When PCOS is well managed, many women:
- Feel more in control of their health
- Spend less time thinking about symptoms
- Have more flexibility in daily life
That’s a meaningful outcome — even without a permanent cure.
You’re Not Failing If PCOS Requires Ongoing Care
Needing continued support doesn’t mean you’ve done something wrong. PCOS management is not a test of willpower or discipline — it’s an ongoing relationship with your body.
Natural strategies, medical care, or a combination of both are all valid paths.
When to Seek Medical Treatment Alongside Natural Approaches
Choosing natural ways to manage PCOS doesn’t mean you have to handle everything on your own. In fact, tFor many women, the most effective and safest approach to PCOS is a combination of lifestyle support and medical care. Knowing when to involve a healthcare provider can help protect your long-term health and prevent unnecessary frustration.
When to Consider Medical Support
- Periods are absent for months
Long gaps between cycles should be evaluated, even if pregnancy isn’t a goal. Medical monitoring helps reduce long-term endometrial risk. - Symptoms aren’t improving or are worsening
Ongoing exhaustion, mood changes, worsening acne or hair symptoms, or persistent cycle irregularity may signal the need for additional support. - Blood sugar or metabolic markers are abnormal
Elevated glucose, insulin, or cholesterol levels require medical guidance to reduce future health risks while continuing lifestyle strategies. - PCOS is affecting mental health
Anxiety, low mood, disordered eating, or feeling out of control deserve professional support as part of comprehensive care. - You’re using supplements or considering hormonal treatment
Medical guidance helps ensure treatments are appropriate, safe, and monitored—especially when combining multiple approaches.
Natural and Medical Care Work Best Together
Natural and medical treatments are not opposites. Medical care provides safety and monitoring, while lifestyle strategies support daily well-being and long-term balance. Using both when needed is often the most supportive approach.
Frequently Asked Questions About Natural PCOS Treatment
How long does it usually take to see results from natural PCOS treatment?
Natural approaches work gradually because they support underlying hormonal and metabolic processes. Some women notice changes in energy, cravings, or mood within a few weeks, while improvements in cycles or skin symptoms often take several months of consistent lifestyle support.
Can PCOS symptoms come back after they improve?
Yes. PCOS symptoms can return if factors like chronic stress, poor sleep, or blood sugar instability resurface. This doesn’t mean treatment failed—PCOS is responsive to lifestyle changes and may require ongoing adjustment over time.
Is natural PCOS treatment effective if I’m not overweight?
Yes. PCOS affects hormone signaling and metabolism regardless of body size. Many women who are lean still benefit from natural strategies that support insulin sensitivity, stress regulation, and hormonal balance.
Natural approaches may help improve acne or hair symptoms over time by supporting androgen balance and reducing inflammation. These changes tend to be gradual and vary from person to person.
Do I need medical supervision when following natural PCOS treatment?
Basic lifestyle changes are generally safe, but medical guidance is important if periods stop for long periods, symptoms worsen, or supplements or hormonal medications are involved. Natural and medical care often work best together.
Is natural PCOS treatment a lifelong commitment?
PCOS management often changes over time. Some strategies may become habits, while others adjust with life stages. Natural treatment is about long-term support, not rigid rules.
Final Thoughts
Managing PCOS naturally is about supporting your body, not fixing it. While PCOS isn’t considered permanently curable, many women find that symptoms become much easier to manage with consistent lifestyle support.
Focusing on blood sugar balance, gentle movement, adequate sleep, and stress regulation can help you feel more stable, energized, and in control over time. Progress doesn’t need to be perfect or linear to be meaningful.
Natural approaches work best when they’re personalized and combined with medical care when needed. With the right support, PCOS doesn’t have to dominate your daily life or limit how well you feel.
References
- Teede, H. J., et al. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(9), 1602–1618.
https://doi.org/10.1093/humrep/dey256 - Azziz, R., et al. (2016). Polycystic ovary syndrome. Nature Reviews Disease Primers, 2, 16057.
https://doi.org/10.1038/nrdp.2016.57 - Moran, L. J., et al. (2013). Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews, Issue 7.
https://doi.org/10.1002/14651858.CD007506.pub3 - Nestler, J. E., et al. (2008). Insulin resistance and ovulatory dysfunction in polycystic ovary syndrome. Endocrine Reviews, 29(6), 777–805.
https://doi.org/10.1210/er.2008-0024 - Thakker, D., et al. (2015). N-acetylcysteine for PCOS: A systematic review and meta-analysis. Obstetrics & Gynecology International, 2015, 1–13.
https://doi.org/10.1155/2015/817849 - Rojas, J., et al. (2014). Polycystic ovary syndrome, insulin resistance, and obesity: Navigating the pathophysiologic labyrinth. International Journal of Reproductive Medicine, 2014, 1–17.
https://doi.org/10.1155/2014/719050
